What is ocular melanosis?
Ocular melanosis is a disease that causes blue, brown or gray discoloration around the iris or on the white of the eye (sclera). It can also cause the iris or the retina to appear darker. It is almost always unilateral (affecting one eye). The condition is typically congenital, meaning it is present from birth. It is also known as ocular melanocytosis.
Ocular melanosis is benign (not harmful) but in rare cases, it can become cancerous.
Ocular melanosis signs
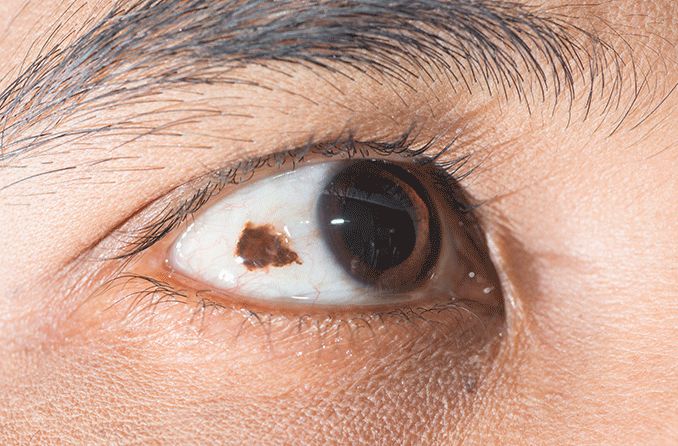
Unilateral lesions of hyperpigmentation are the main feature of ocular melanosis. A lesion is an area of tissue that has developed abnormally. Lesions can be cancerous (malignant) or, in the case of ocular melanosis, non-cancerous (benign). Hyperpigmentation occurs when too much melanin is made, creating spots of discoloration.

Credit: "Primary acquired melanosis" from the University of Iowa is licensed under CC Attribution 3.0 Unported.
Melanocytes are the cells responsible for creating melanin. Melanin is what gives color to hair, eyes and skin. The more melanin is present in an area, the darker the color of that area.
Ocular melanosis may appear as partial heterochromia, the presence of more than one color in the iris of the eye. It may also show up as gray or bluish spots on the sclera. It can also affect the choroid - the layer on the inside of the eye that is between the sclera and the retina (the nerve tissue at the back of the eye) and will make the retina appear darker. The majority of cases only appear in one eye (unilateral).
Causes of ocular melanosis
At this point, there is no known cause of ocular melanosis. The lesions are most often present at birth. However, a person can also develop them during puberty or while pregnant. This is likely due to hormonal shifts that occur during these periods.
Who gets ocular melanosis?
Ocular melanosis is a rare condition. It is more common in females, particularly those of Asian or African descent. It is less common for Caucasians to develop ocular melanosis. However, those who do have a much higher risk of subsequently developing cancer.
How is ocular melanosis diagnosed?
An eye doctor can perform a few different exams in order to diagnose ocular melanosis. These include:
Slit lamp exam
A slit lamp is a microscope with a bright light. It allows providers to see the layers on top of and inside the eye. This can help locate the hyperpigmentation to verify if it is on the sclera (the white of the eye) or the conjunctiva (the layer on the outer surface of the eye).
Gonioscopy
People with ocular melanosis have an increased risk of developing glaucoma. Because of this increased risk, their eye doctor will likely perform a gonioscopy.
This test involves a slit lamp and prisms to allow the provider to look at the drainage angle of the eye. The drainage angle is what allows fluid in the eye to drain properly. Gonioscopy is particularly helpful in distinguishing what type of glaucoma an individual has.
Dilated ophthalmoscopy
Ophthalmoscopy is an exam an eye doctor may perform to look at the fundus (the back part of the eye). An ophthalmoscope, a handheld instrument with lenses and a bright light, allows the provider to see the optic nerve. They may dilate (widen) the pupils with eye drops first in order to get a better view.
Dilated ophthalmoscopy will help the provider look for signs of glaucoma. It can also help them look for hyperpigmentation on the choroidal layer.
Ophthalmic ultrasound
An eye doctor may perform an ophthalmic ultrasound to examine the uveal layer of the eye. This layer contains:
- The iris – The colored part of the eye
- The choroid – The layer of blood vessels
- The ciliary body – A layer of muscle that helps change the shape of the eye’s lens
An ophthalmic ultrasound uses sound waves to create an image of the inner structure of the eye. This exam can help the doctor look for signs of uveal melanoma.
Dermoscopy
In cases where the hyperpigmentation may also be on the skin and/or eyelids, a dermoscopy may be useful. A doctor will use a dermatoscope, a magnifying glass with a very strong light, to look at the structure and color of the skin. This helps them get a better view of the pigmented lesions.
What looks similar to ocular melanosis?
Several conditions have signs and symptoms similar to ocular melanosis, including the following:
Ocular melanosis vs. ocular melanoma
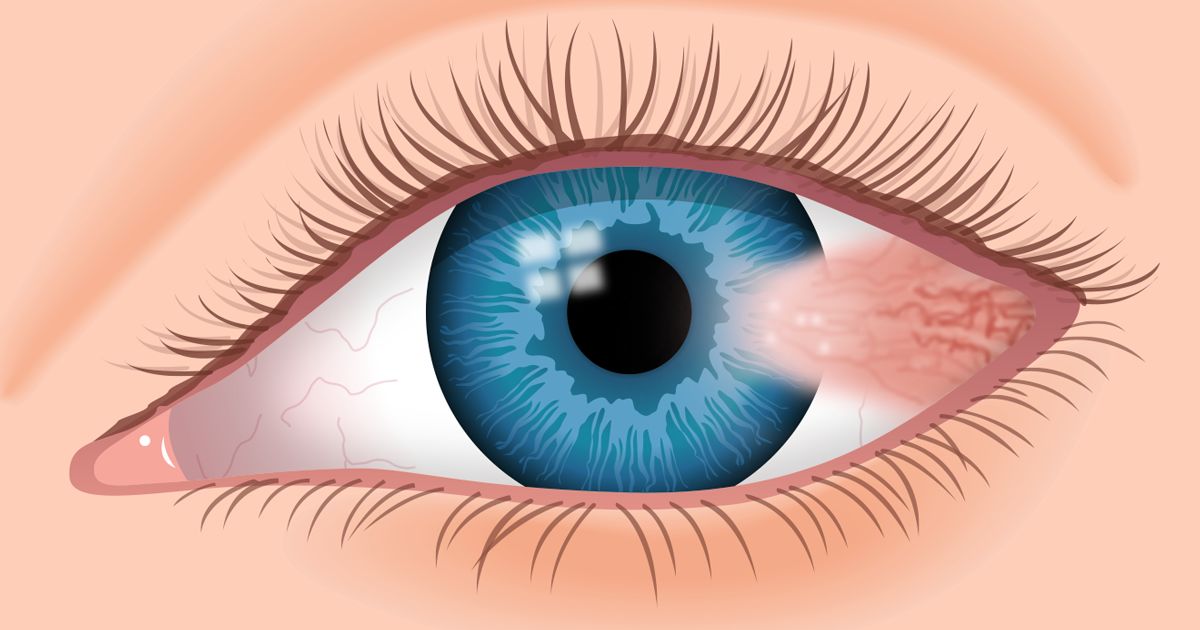
Ocular melanoma is a rare form of cancer that develops in the eye’s melanocytes, the cells that create melanin. It usually starts in the uvea, a hidden layer inside the eye that contains the most pigment, but it can also, rarely, develop on the iris or the conjunctiva.
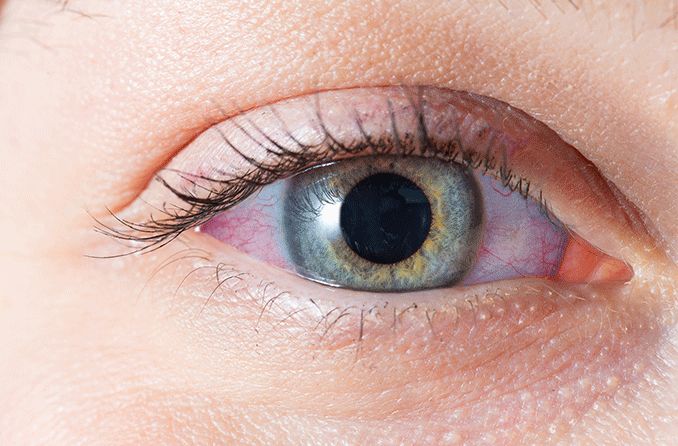
While ocular melanosis is visible on the surface of the eye, ocular melanomas usually form inside the eye where they cannot be seen in a mirror. There is also a chance they will be asymptomatic, meaning they don’t trigger any obvious warnings. However, ocular melanomas can lead to loss of vision and glaucoma, and they can even metastasize (spread to other areas of the body).
When ocular melanosis affects the conjunctiva it is flat, with an even distribution of pigment, and does not grow in size. Contrarily, melanoma of the conjunctiva does grow, is usually raised, more darkly pigmented with variable pigmentation, and often has thick blood vessels around it (called feeder vessels).
Like ocular melanosis, there is no known cause for ocular melanoma.
Ocular melanosis vs. nevus of Ota
Nevus of Ota, or oculodermal melanosis, is a form of ocular melanosis that appears on the eyelid as well as the eye itself. Those with nevus of Ota have a one-in-10 risk of developing glaucoma and a one-in-400 risk of developing melanoma of the surface and inside of the eye.
Other conditions similar to ocular melanosis
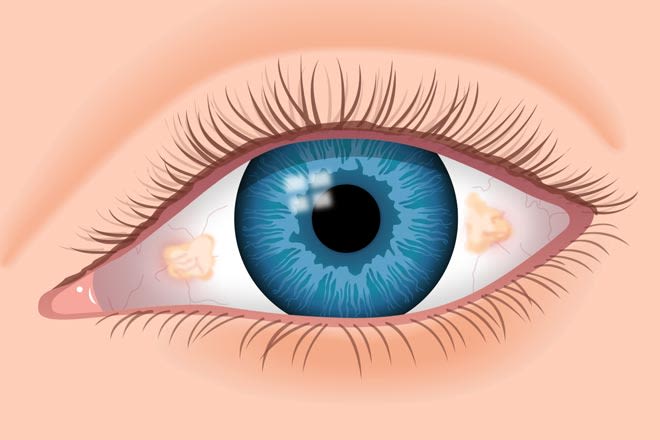
- Freckle of the conjunctiva – Usually unilateral, slightly raised with small fluid pockets (cysts). It is typically present since childhood but may change during puberty or pregnancy. This almost never turns into melanoma.
- Complexion-associated melanosis – Usually bilateral (in both eyes), flat without cysts and with fuzzy borders. More common in darkly pigmented individuals, it becomes more visible with age. This is the most common type of pigmentation of the conjunctiva and it does not turn into melanoma.
- Primary acquired melanosis – Unilateral, flat without cysts and patchy, it may be present on the cornea. This is thought to be a subtype of ocular melanosis that has a higher risk of turning into melanoma. A danger sign is if the size of the spot fluctuates over time.
READ NEXT: What Is Ochronosis
Ocular melanosis treatment
Because ocular melanosis is not harmful, no treatment is required. However, regular checkups are encouraged. Individuals with ocular melanosis or nevus of Ota are at higher risk for developing glaucoma or melanoma.
Glaucoma
Glaucoma occurs when fluid builds up in the eye. This creates pressure that can damage the optic nerve. When not properly treated, glaucoma can cause blindness. Treatment options include prescription eye drops and laser surgery.
Ocular melanoma
Ocular melanomas can be treated through radiation or surgery. Treatment will depend on the size and location of the cancer, as well as the health of the patient.
When ocular melanosis has been present in the eye for a long time, especially since early childhood, it is much less likely to be melanoma. In the case of oculodermal melanosis or primary acquired melanosis, the risk of melanoma is much increased.
READ MORE: Ocular Melanoma Awareness Month
When to see a doctor
If you notice discoloration on or around your eyes, you should have them checked regularly. Your eye doctor will monitor any eye pressure changes that may indicate if glaucoma has developed.
It is also important to monitor any changes in the size or shape of lesions that have developed. If a lesion grows or changes shape, it could be a sign that the spot has become cancerous.
SEE RELATED: Orbital pseudotumor