Schizophrenia and your eyes
Visual impairment likely isn’t the first thing people think of when they think of schizophrenia. However, schizophrenia and the medications prescribed for it often impact visual processing. Patients may experience visual hallucinations, involuntary eye movements and other visual symptoms.
Scientists are still unsure how many of these symptoms start in the eyes and how many start in the brain.
What is schizophrenia?
Schizophrenia is a mental disorder. It can impair emotional management, decision making and ability to relate to others. It is often characterized by negative symptoms, delusions and cognitive impairment. Schizophrenia impacts between 0.25% and 0.64% of adults in the U.S.
There are several potential factors that can lead to schizophrenia, including:
- Genetics
- Environment
- Brain chemistry
- Substance use
Schizophrenia and the eye
Schizophrenia and its treatment can lead to physical changes to the patient’s eyes. The retina — the tissue lining the back of the eye — develops from the same tissue as the brain. This means that changes to the brain’s structure or function may also impact the retina.
The retina turns light into nerve signals, which the brain interprets as “vision.” Any changes or damage to the retina can lead to significant visual impairment.
This link between the brain and the retina may someday help physicians assess risk for mental disorders through eye exams. For example, some studies are investigating a possible link between increased vein width in the retina and psychosis.
There are several visual symptoms that have been associated with schizophrenia. But it is essential to emphasize that having these symptoms does not mean an individual has schizophrenia. Additionally, many changes to vision and the eyes are not due to the condition, but the medications that are taken to treat the condition.
Nystagmus
Nystagmus occurs when the eyes involuntarily move, typically in a repetitive manner. These movements may be side-to-side, up-and-down or circular. Some past studies estimate around 50% to 85% of people with schizophrenia are estimated to experience nystagmus.
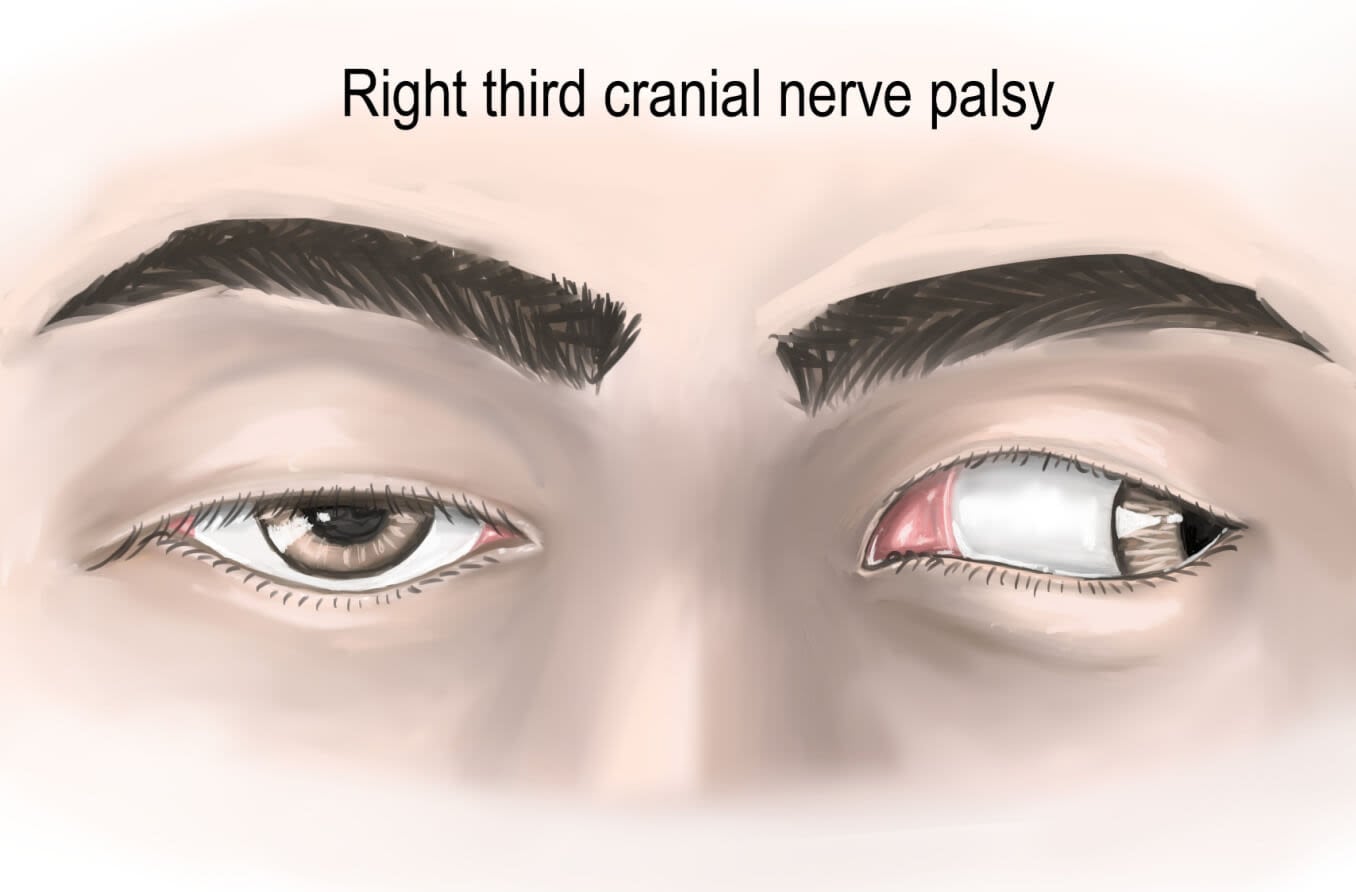
Strabismus
Strabismus is a condition in which the eyes look in two different directions. It occurs when the muscles surrounding the eyes stop working together. This causes the eyes to see different images, which, in turn, can confuse the brain. Over time, the brain may start to ignore the image sent by the weaker eye. If not treated, that eye may never see well, creating a “lazy eye” (amblyopia).
Like nystagmus, strabismus can be congenital or develop later in life. A 2004 study of approximately 350 people with schizophrenia found that strabismus — specifically, a constant turning out of one eye — was present in around 13% of the group. Later studies also reported similar findings. Experts continue to investigate whether there may be a link between childhood strabismus or amblyopia and increased risk of schizophrenia.
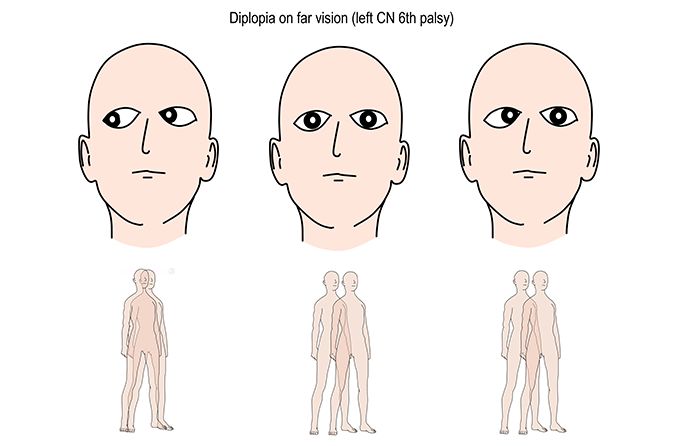
Smooth-pursuit eye movements (SPEM)
Smooth-pursuit eye movements are how the eyes follow objects that are in motion. SPEMs are typically slow and steady. However, individuals with schizophrenia may demonstrate smaller, jerkier eye movements.
SPEMs can be tested using an antisaccade task. Saccades are eye movements that shift the center of focus from one object or area to another. They are quick movements that can be voluntary or involuntary.
The antisaccade task asks individuals to focus on a dot. When another dot appears, the individual is asked to intentionally look in the opposite direction. The test measures their ability to control their natural visual reflex by not looking at the new dot.
In some studies, individuals with schizophrenia were found to have difficulty with smooth-pursuit eye movements.
Impaired visual acuity
The link between psychiatric disorders like schizophrenia and impaired vision is fairly well established. However, the reason for this link is still up for debate.
There are some potential causes to be explored:
- Individuals with psychiatric disorders may struggle to make and keep eye appointments. This can lead to further impairment if visual issues are not addressed.
- Psychiatric disorders increase the chance of developing diabetes or cardiovascular issues. Some of the medications for psychiatric disorders can also increase this risk. Diabetes and cardiovascular disease can damage the eyes and lead to visual impairment.
- Antipsychotic medications can cause blurred vision.
- Aberrant (abnormal) visual input may cause an individual to develop a psychiatric disorder.
Schizophrenia and color vision
The neurotransmitter dopamine plays a role in both brain function and retinal function. Neurotransmitters are chemical messengers that run throughout the body. In the brain, dopamine acts as a reward system for enjoyable activities. In the retina, dopamine plays a major role in the eye’s ability to adjust to different levels of light.
There are two main types of dopamine receptors — sites it can attach to — in both the retina and the brain: D1 and D2. It is hypothesized that, when the second type (D2) overacts, it can contribute to schizophrenic symptoms like hallucinations. This overactivity in the retina’s second dopamine receptor may also cause hyper-intense color vision.
Schizophrenia and hallucinations
Among the most commonly associated symptoms of schizophrenia are hallucinations. Hallucinations involve an individual’s perception of something that others cannot perceive. This may be a sight, sound or smell. Hallucinations can lead to distress and confusion because they seem very real to the individual perceiving them. For individuals with schizophrenia, auditory (sound-related) hallucinations are most common. However, visual hallucinations may also occur.
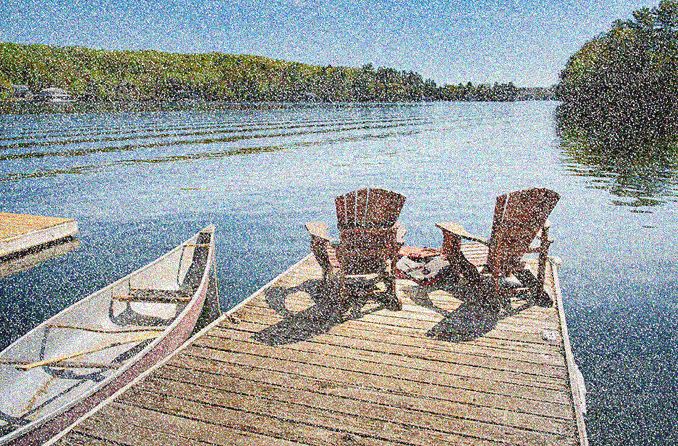
In some cases, visual hallucinations involve seeing things that aren’t really there. In others, they involve seeing objects with some kind of distortion. For individuals with schizophrenia, in addition to dopamine, glutamate may play a role in hallucinations.
Glutamate plays a role in learning, memory and relaxation. In the eye, it is released by photoreceptors and other cells found in the retina. Photoreceptors are cells in the retina that convert light into nerve signals, which are then sent to the brain. They are responsible for color vision and low-light vision.
Some experts have speculated that glutamate abnormalities in the eye may play a role in visual symptoms associated with schizophrenia, such as visual distortions and hallucinations.
When to see a doctor
Eye doctors are not able to diagnose schizophrenia, but annual eye exams are still crucial. Individuals with schizophrenia are at higher risk for some eye conditions that can lead to visual impairment.
Many individuals with schizophrenia have difficulty recognizing that they need medical attention. If a loved one is exhibiting symptoms of schizophrenia, you may need to encourage them to seek help.
Individuals with schizophrenia can have a higher risk of suicidal thoughts and behaviors. If you are concerned about a friend or loved one, there are a few options:
- Call 911 or your local emergency number
- Contact the National Suicide Hotline at 800-273-TALK (8255)
- If you can do so without risk to the individual or yourself, take them to the nearest hospital