Understanding retinal detachment
Retinal detachment is a serious eye condition that occurs when a portion of the retina lifts away or becomes separated from the back of the eye. The condition, also referred to as a detached retina, is a medical emergency that requires prompt care.
The retina is the light-sensing membrane located in the back of the eyeball. It is responsible for detecting light and sending those signals to the brain, which processes the images we see. When the retina becomes detached from the eyeball, it cannot function properly, which impacts vision.
Any amount of retinal detachment generally affects vision in some way. If the condition is not diagnosed and treated promptly, permanent vision loss and even blindness may occur. This is what makes a detached retina an emergency situation.
While the condition commonly affects one eye, it may affect both in rare cases.
Causes and risk factors
There are various types of retinal detachment, each of which may develop due to different factors. The more common causes and risk factors are discussed below.
Common causes of retinal detachment
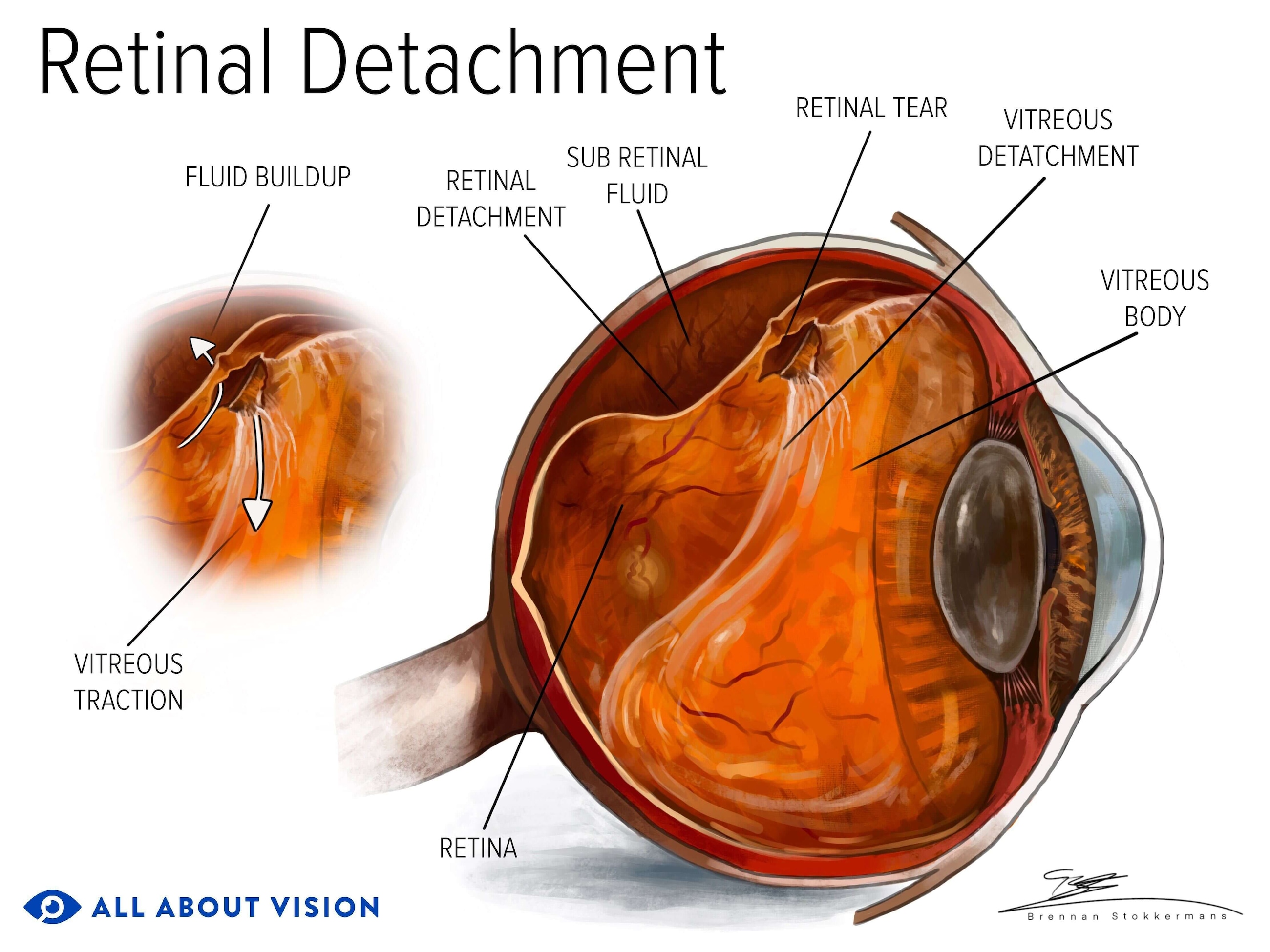
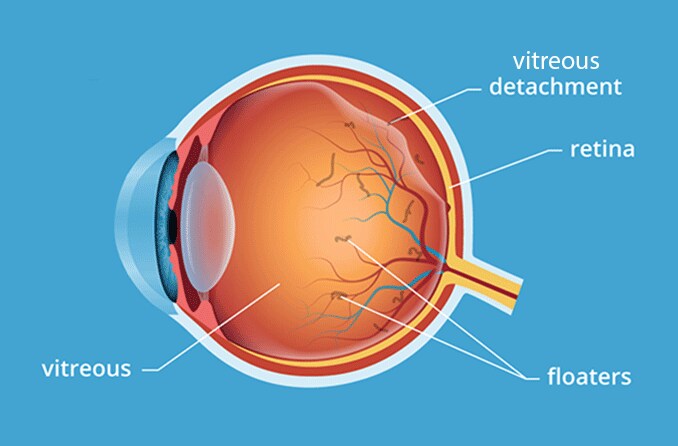
In its normal position, the retina is located next to the vitreous humor, which is a gel-like substance that fills the center of the eyeball. As people age, the vitreous becomes more liquid in consistency. It may shrink and pull away from the retina. This is called posterior vitreous detachment.
In most cases, this process occurs without issue. But in others, this separation can tug on the retina and cause it to tear. When the retina tears, fluid may leak into the space behind the retina, causing it to peel away from the back wall of the eye. A detached retina is partially cut off from the blood supply and nourishment it needs for health. As a result, vision loss occurs.
While a detached retina is commonly caused by a retinal hole or tear, it may also be caused by:
- Retinal trauma or injury
- Retinal neovascularization (growth of abnormal blood vessels)
- Proliferative membranes on the retina or vitreous (growth of a fibrous membrane)
- Scar tissue development on the retina
- Fluid buildup on or beneath the retina
A variety of conditions may contribute to these retinal detachment causes.
Who is at greater risk?
Age is a risk factor for retinal detachment. The condition can impact a person at any age, but it is more common in those who are middle-aged or older. Males may also be more likely than females to experience a detached retina.
Other retinal detachment risk factors include:
- Myopia (nearsightedness)
- High myopia (extreme nearsightedness)
- Retinal tears
- Retinal holes
- Posterior vitreous detachment
- Family history of retinal detachment
- History of surgery for cataracts or other eye conditions
- History of retinal detachment in the opposite eye
- Trauma to the eye or head
- Peripheral retinal degeneration
- Diabetes and diabetic retinopathy
- Occupational heavy lifting
- Glaucoma
It is important to maintain regular eye exams, especially if you have one or more of the retinal detachment risk factors listed above. Regular eye exams can allow eye doctors to spot the signs of a detached retina as early as possible.
Key symptoms of retinal detachment
Identifying the early signs and symptoms is key to getting a prompt diagnosis and treatment. This can help prevent the retina from further tearing or detaching.
A detached retina usually does not cause pain. Some cases may not cause any symptoms, but this is very rare.
Early warning signs and symptoms
Symptoms of a detached retina may occur abruptly or increase suddenly. When visual retinal detachment symptoms are present, they may include:
- Flashing lights (similar to “seeing stars”)
- Dark spots in your vision
- Eye floaters (especially the presence of new floaters)
- Sudden blurred vision (in one eye)
- Loss of peripheral (side) vision
A smaller retinal detachment may carry no early symptoms at all. However, it is just as concerning as one that causes symptoms. An eye doctor can see the early signs of a detached retina during a routine eye exam, even if you haven’t noticed vision changes.
These symptoms may also occur with other conditions. If you experience a sudden vision change or any other symptoms, contact your eye doctor immediately.
Progression of symptoms
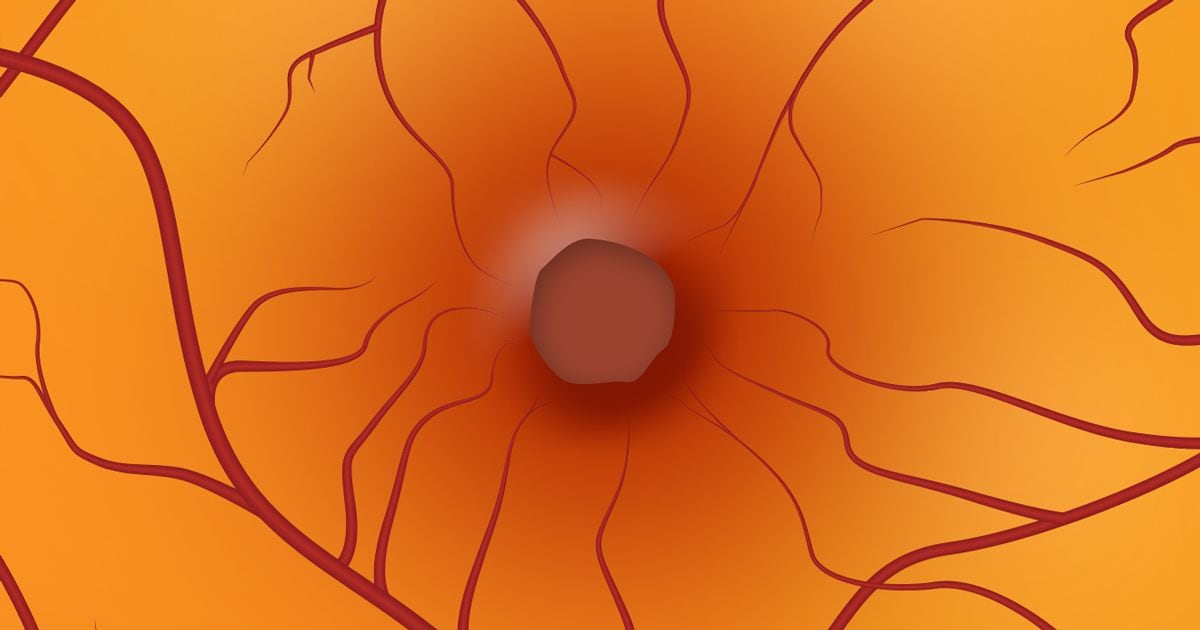
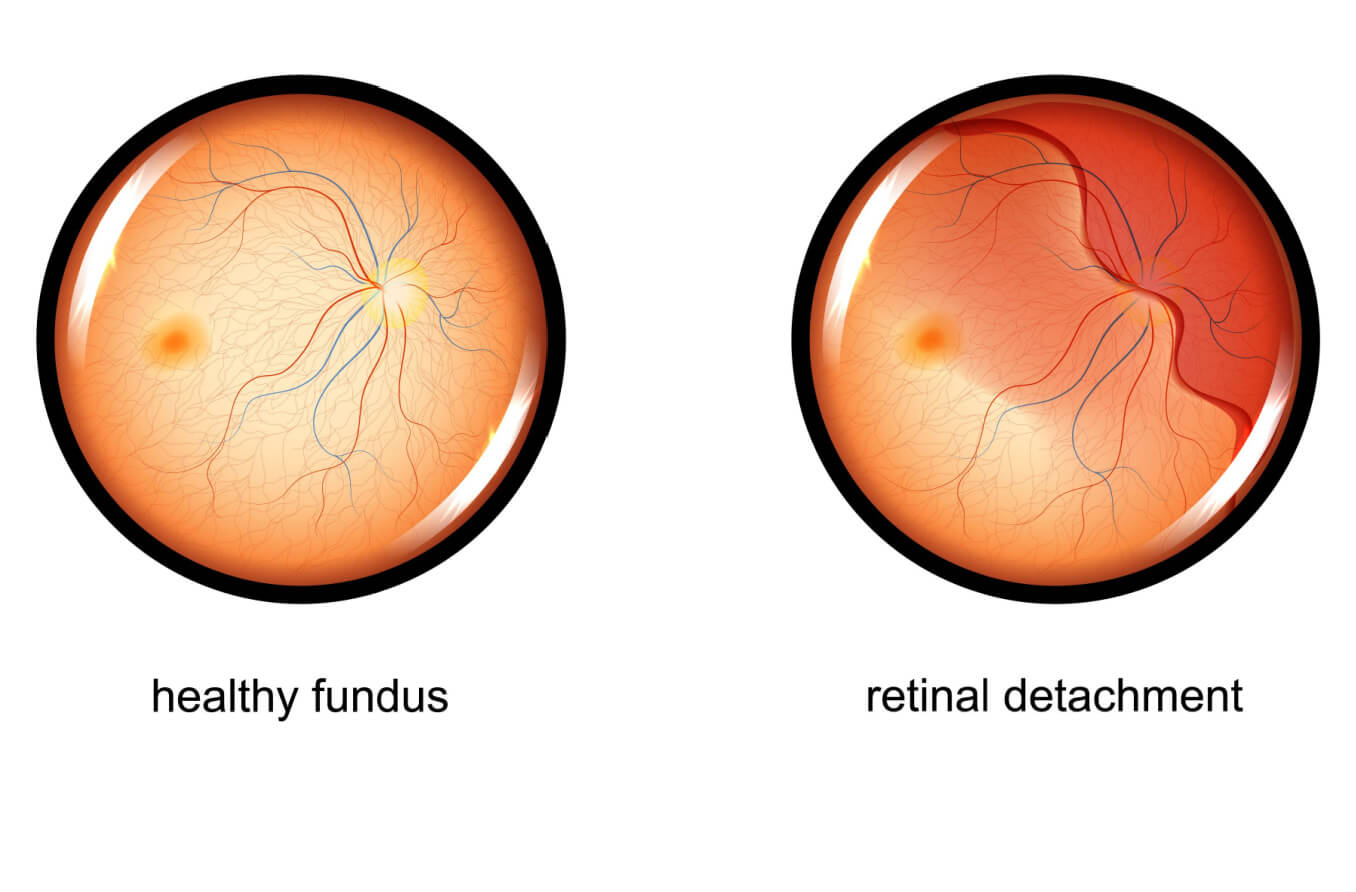
Retinal detachment symptoms may vary based on where the detachment is located. For instance, if the portion of the retina that contains the macula becomes detached, central vision loss occurs. The macula, located in the center of the retina, helps you see objects in front of you in sharp, clear detail. When the outer parts of the retina are affected, a gray shadow or curtain may impact your side vision.
Vision loss may begin in the outer areas of your field of view. It may be stable (unchanging), or it may slowly get worse. The presence of a gray shadow or curtain in your vision often indicates that the condition is progressing.

Seeing a curtain-like shadow coming down across your field of vision can be a sign of retinal detachment.
Floaters, flashes and changes in vision
Most often, flashes and floaters in your vision are harmless. They are a common part of aging and generally not a cause for concern. Floaters resemble lines, tiny dots or cobwebs that drift into your view. Flashes are more like arcs of light, lightning or the sensation of “seeing stars.”
However, eye flashes and floaters can also indicate a torn retina or retinal detachment. If you notice a sudden increase in flashes or floaters, or a gray curtain or shadow in your field of vision, contact an eye doctor as soon as possible. The earlier you get treatment for a torn or detached retina, the greater the chance of preserving your vision. The likelihood of permanent vision loss generally increases the more time that passes.
Even minor vision changes can be a major cause for concern. It is important to see an eye doctor promptly when any change in your vision occurs.
SEE RELATED: Retinal vasculitis: Causes, symptoms and treatments
Types of retinal detachment
There are two main types of retinal detachment: rhegmatogenous (reg-mah-TAH-jeh-nus) and non-rhegmatogenous. The non-rhegmatogenous form is further broken down into two subtypes, which include tractional and exudative detachments.
The primary difference between rhegmatogenous and non-rhegmatogenous detachments is whether or not they involve a tear or “break” (rhegma) in the retinal tissue.
All types of retinal detachment can lead to permanent vision loss and even blindness.

Rhegmatogenous retinal detachment
The most common type of retinal detachment is the rhegmatogenous form. It generally results from retinal tears or holes (such as a macular hole) due to posterior vitreous detachment or from eye injury or trauma. Retinal tears allow vitreous fluid to seep into the area behind the retina, causing the retina to separate from the back of the eye.
Rhegmatogenous retinal detachments (RRDs) are caused by posterior vitreous detachment in 80%-90% of cases. Men may be more prone to develop RRDs than women. While anyone can be affected by this type of detachment, it is often associated with:
- Aging
- Nearsightedness (myopia)
- Eye trauma or injury
- Heavy lifting
- Breakdown of vitreal and retinal tissues (such as in lattice degeneration)
The rate at which a rhegmatogenous retinal detachment develops varies and can range from a few hours to several months. This is dependent on where the detachment takes place. RRDs tend to develop more quickly than other types of detachments.
Tractional retinal detachment
Tractional retinal detachments (TRDs) develop when scar tissue forms and tugs or pulls on the retina. When this “traction” causes too much tension, the retina can detach from the back of the eye. Scar tissue may develop when new, abnormal blood vessels form in or around the retina. It may also occur due to fluid accumulation on the surface of the retina.
Diabetes mellitus, leading to diabetic retinopathy, is the most common cause of this type of detachment. It can also be caused by sickle cell disease and other conditions that lead to the growth of new, abnormal vessels in the retina.
In some instances, TRDs may develop due to retinal scarring caused by trauma or following RRD surgery.
Symptoms may not be noticeable during the early stages of a TRD.
Exudative retinal detachment
Exudative retinal detachments (ERDs), also called serous retinal detachments, develop when fluid leaks into the space beneath the retina. This fluid accumulation may result from a dysfunction of the blood–retinal barrier (BRB). The BRB helps regulate the flow of blood and fluids within the retina.
The buildup of this fluid causes separation of the retinal layers, lifting the retina away from its normal position in the back of the eye.
ERDs may be caused by a wide range of factors, including:
- Infectious diseases
- Inflammatory conditions
- Tumors in the retina or choroid (the layer between the retina and sclera)
Other eye-related conditions may also increase the risk of ERDs. These include age-related macular degeneration, Coats’ disease and retinal vein occlusion, among others.
Symptoms may not be apparent in the early stages of an ERD.
Diagnosing retinal detachment
Retinal detachment diagnosis generally begins with a comprehensive eye exam. Some people may seek an eye exam due to detached retina or retinal tear symptoms. However, asymptomatic cases might only be identified during regular eye visits. Since some cases of retinal detachment may not show symptoms, it is important to have annual eye exams to screen for retinal and other eye concerns.
Clinical examination methods
During the exam, your eye doctor may first evaluate the front part of your eye through a slit-lamp examination. They may also assess your visual acuity, color vision, eye pressure and other factors. Your doctor will then place special eye drops in your eyes to dilate (widen) your pupils. This helps them see your retina and determine if a detachment or other damage may have occurred.
Once your eyes are dilated, your eye doctor may perform a fundoscopic exam, or ophthalmoscopy, to evaluate the back part of your eye (fundus). One or more of the following techniques may be used:
- Direct ophthalmoscopy – Performed with a handheld device called an ophthalmoscope that is similar to a flashlight
- Indirect ophthalmoscopy – Performed with an ophthalmoscope device worn on the doctor’s head
- Slit-lamp ophthalmoscopy – Performed with the use of a slit-lamp microscope
Each technique involves a bright light and special lenses the doctor uses to see the retina and surrounding structures.
Imaging and advanced diagnostics
Retinal imaging and scanning may also be performed to provide your doctor with a better view of your retina. This may include:
- Optical coherence tomography (OCT) – A technique that captures images of the retina using light-wave technology
- Ophthalmic ultrasound – A technique that captures images of the eye (including the retina) using sound waves
- Computed tomography (CT) scan – A technique that captures 3D images of the eye (including the retina) using radiographic technology
- Magnetic resonance imaging (MRI) – A technique used to capture detailed images of the eye (including the retina) using a magnetic field and radio waves
- Wide-angle retinal photography – A technique that aids the doctor in visualizing a broader area of the retina
If a detached retina is detected, your eye doctor may refer you to a retina specialist. A retina specialist is an ophthalmologist who has advanced training in the diagnosis, treatment and management of retinal diseases.
Treatment options for a detached retina
A detached retina generally will not resolve on its own and usually requires prompt care. In very rare cases, it may reattach and heal without intervention. However, most cases need immediate treatment to prevent further damage and preserve vision.
Treatment to repair a detached retina depends on the type and severity of detachment that has occurred. All treatment options for the condition are surgical, but some are a little less invasive. The type of retinal detachment surgery performed may depend on the underlying cause.
Noninvasive surgical interventions
Detached retinas caused by small retinal tears are often treated through a noninvasive surgical approach. This type of retinal detachment treatment typically seals or repairs the tear and reattaches the retina to the back of the eye. Noninvasive retinal detachment surgery can include:
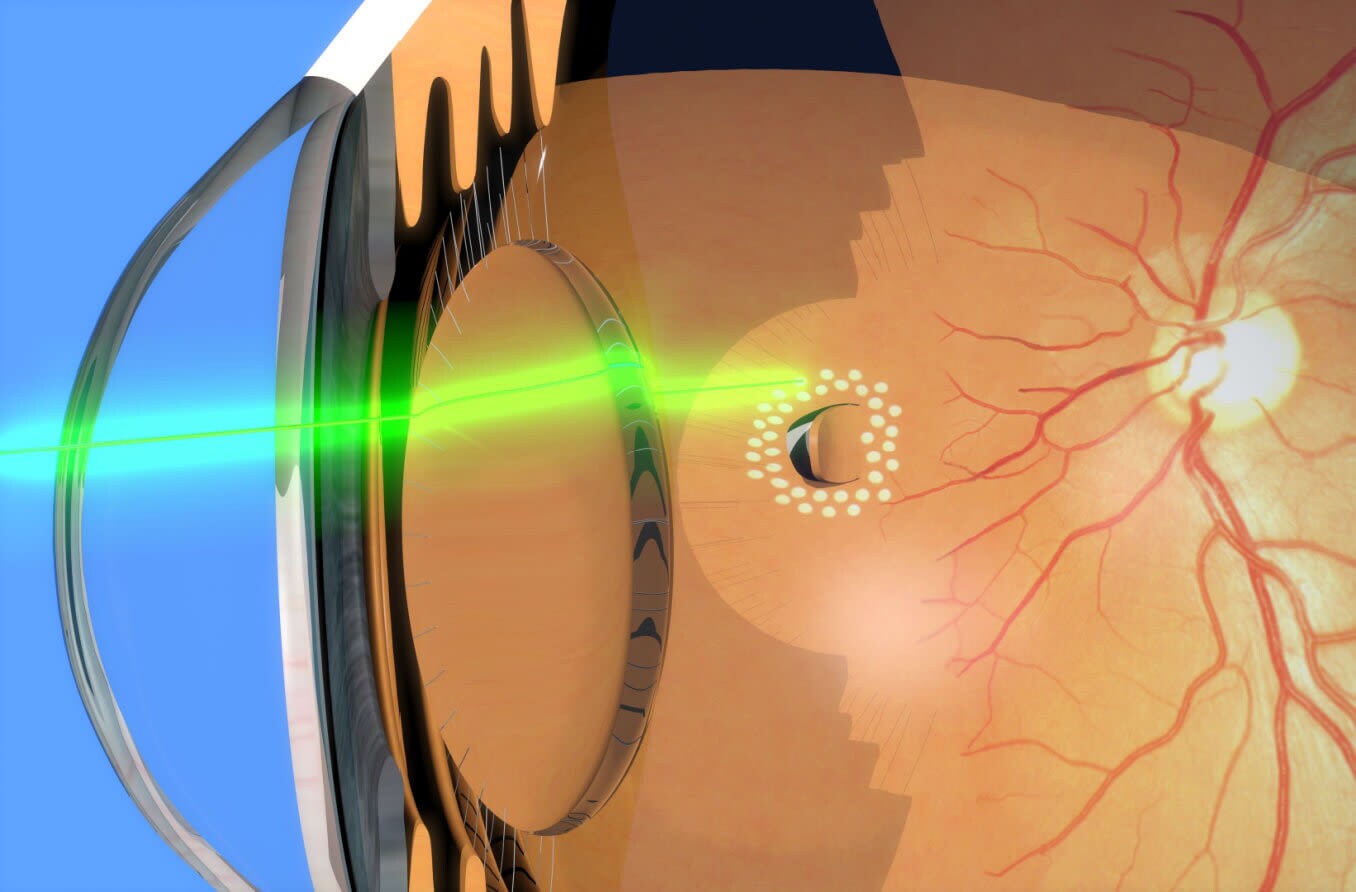
Laser photocoagulation (LPC)
LPC uses laser heat to create scar tissue in the treatment area. The scar tissue reconnects the torn tissues to seal off the opening and reattach the retina to the eye wall.
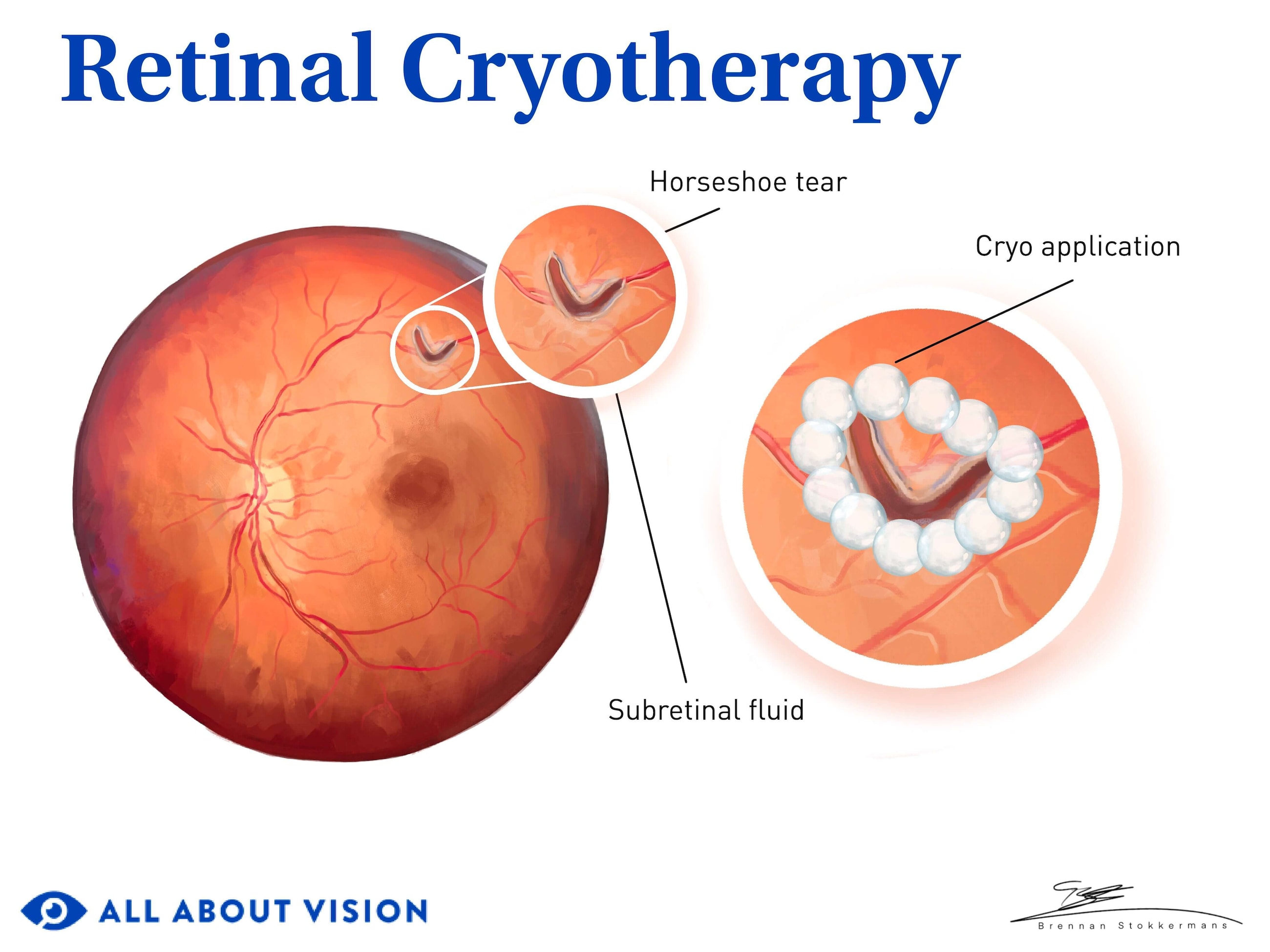
Cryopexy (freezing)
Cryopexy uses cold energy produced by a probe. The extreme cold creates scar tissue in the area of the tear to seal it off and reattach the retina to the back of the eye.
Additional surgical procedures
In more advanced cases of retinal detachment, other surgical procedures may be necessary to repair the damage. These retinal detachment treatments may include:
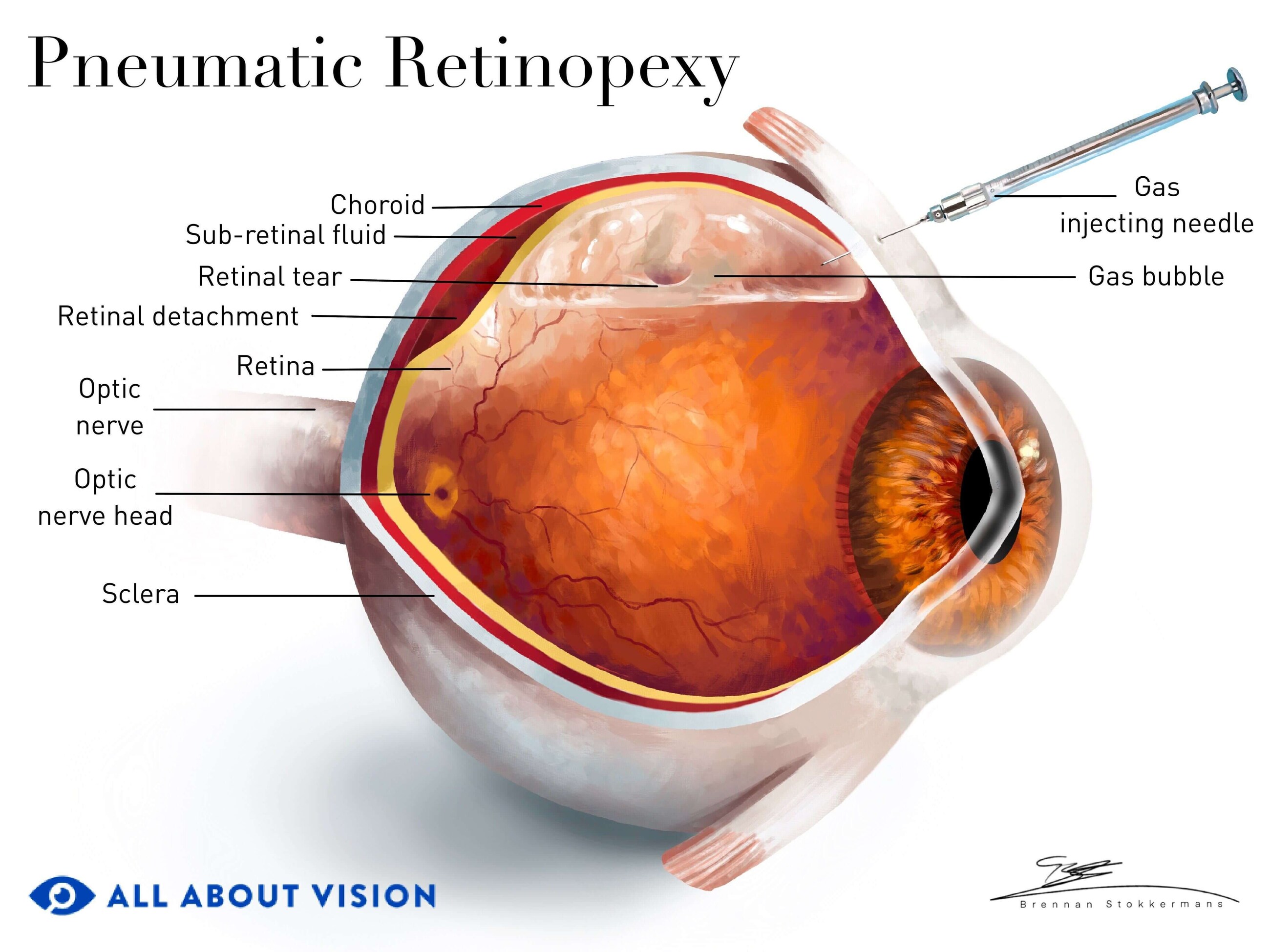
Pneumatic retinopexy
During this procedure, a gas bubble is injected into the eye. The bubble pushes the detached portion of the retina back into place.
You will need to keep your head in a certain position, for a specified period of time, following the procedure. This will help to keep the gas bubble in place and allow your retinal tissues to heal. The natural production of fluid within your body will eventually replace the bubble to help keep your retina in place.
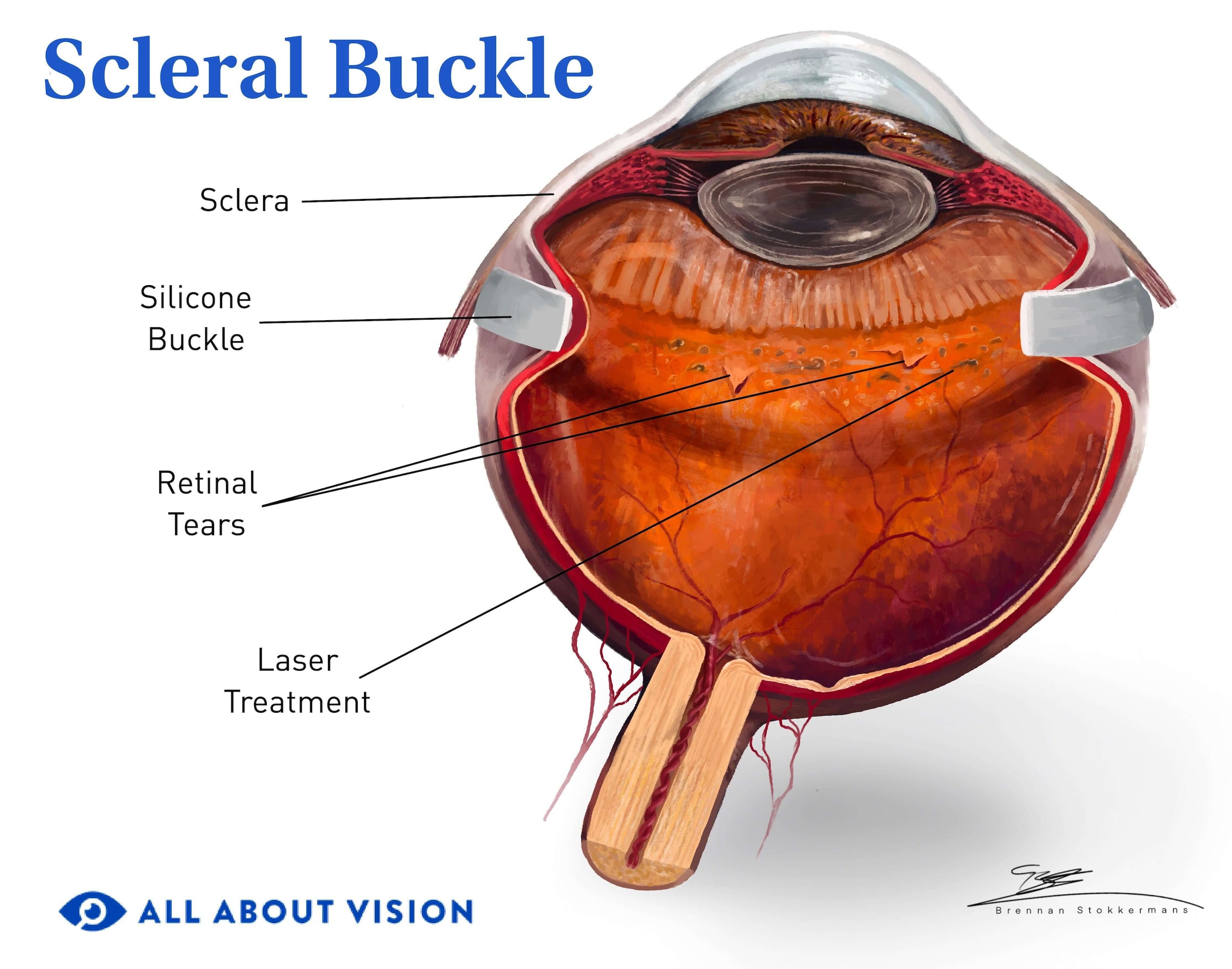
Scleral buckling
With scleral buckling, a plastic or rubber band is placed on the outer wall of your eye (sclera), encircling the eye. The band helps push the retina back into place, allowing it to heal and reattach to its proper location.

Vitrectomy
A vitrectomy removes the portion of the vitreous humor that is tugging on the retina and causing it to detach. A bubble of oil, gas or air is then positioned where the vitreous was removed. This helps keep the retina in its proper position as it heals and reattaches to the eye wall.
Retinal detachment recovery
The retinal detachment recovery process varies depending on the type of procedure performed. Your eye doctor will tell you what to expect during the treatment process. They will also provide aftercare instructions, such as whether medication is needed or if an eye patch should be worn.
If an air or gas bubble was placed during the procedure, you may be advised to avoid certain forms of anesthesia and activities, such as diving or flying, for a certain period of time. You may also need to keep your head in a specific position for up to one to two weeks, per your doctor’s recommendation.
READ MORE: Recovering from retinal detachment surgery
Prevention and reducing risks of retinal detachment
You may not be able to prevent a retinal detachment, especially when it occurs due to age or if you have a genetic predisposition. However, understanding the warning signs and when to seek care is an important first step in preventing further damage.
If you notice any retinal detachment symptoms or experience trauma or injury to your eyes, seek medical care right away. Prompt treatment is essential to reduce the risk of permanent vision loss. Having a retinal hole or tear repaired also helps prevent a full-blown detachment from occurring.
Lifestyle and dietary recommendations
There are certain steps you can take to help with retinal detachment prevention. These lifestyle precautions may lower your risk of the condition:
- Protect your eyes – Wearing polycarbonate lenses or goggles can prevent injury to the eyes during sports or activities that place your eyes at risk of impact.
- Control diabetes and blood sugar levels – Diabetic diseases are a risk factor for the condition. Controlling your blood sugar could help reduce your chance of experiencing a detached retina.
- Avoid heaving lifting – The lifting of heavy objects associated with certain occupations is a risk factor for some individuals. Taking steps to use proper ergonomics and assistance may help lower the chance of retinal detachment.
- Monitor your diet – Following a healthy diet may reduce the risk of eye conditions like diabetic retinopathy, which is a risk factor for retinal detachment. Taking certain nutritional supplements may provide some benefits as well. Your doctor can help you determine if dietary modifications or supplements may be right for you.
- Maintain a healthy lifestyle – Getting plenty of exercise and maintaining a healthy weight can also lower the chance of diabetic retinopathy. A healthy lifestyle helps support your general eye health.
Regular eye examinations
Getting annual eye exams helps reduce your risk of vision loss due to retinal detachment. Regular exams allow your eye care professional to catch signs of a retinal condition as early as possible, often even before symptoms occur. They can monitor the health of your eyes and help you evaluate your potential risks for retinal or other eye diseases.
Your doctor may recommend having your eyes examined more often if you have a higher chance of developing the condition.
Once again, a detached retina is an emergency situation. If you experience symptoms of this condition or have any other vision changes, see your eye doctor as soon as possible.
READ NEXT: Detached retina FAQs