What is retinal vasculitis?
Retinal vasculitis (RV) is characterized by inflammation in the retina’s blood vessels. Although it is not painful, it does cause vision loss. Some cases of RV may be the result of inflammatory or infectious disease elsewhere in the body. Other cases may be localized to the eye.
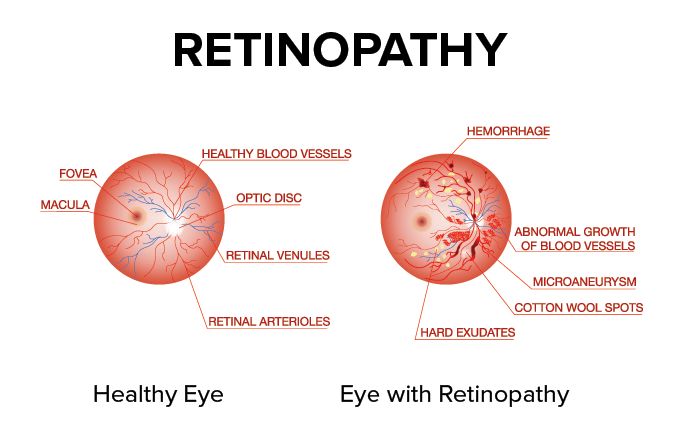
Vasculitis is a condition in which blood vessels become inflamed. The cause of this inflammation is often unknown. Blood vessels are responsible for blood delivery throughout the body. They consist of:
Veins – tubes that carry blood to the heart
Arteries – tubes that carry blood from the heart to the rest of the body
Capillaries – small tubes that connect the veins and arteries
Inflammatory responses are usually the result of an injury, infection or the body’s immune system attacking its own tissue (auto-immune reaction). Retinal vasculitis is an auto-immune reaction against retinal blood vessels.
What are the types and causes of retinal vasculitis?
Retinal vasculitis can be one of two types: primary or secondary. Primary RV is when the immune system specifically targets the body’s blood vessels. Secondary RV is when the immune system does not specifically target the body’s blood vessels, but they do get inflamed.
Both primary and secondary RV can affect the eye only or affect blood vessels elsewhere in the body as well.
Primary retinal vasculitis
Primary RV can occur with no known cause. However, there are some conditions that can directly lead to this type of RV.
Some causes of primary retinal vasculitis are specific to the eye:
Uveitis – inflammation of the uvea, which consists of the iris, the ciliary body and the choroid.
Frosted branch angiitis – a rare condition that causes vascular inflammation throughout the retina. The inflammation can cause white sheathes to develop around the vessels. This makes them look like frosted tree branches.
Idiopathic retinal vasculitis, aneurysms and neuroretinitis (IRVAN) – a rare inflammatory condition. It causes RV, abnormal widening of the arteries and optic nerve inflammation. The cause of IRVAN is unknown.
Pars planitis – an idiopathic inflammatory condition. It is a form of uveitis that mostly appears in children and teens. The inflammation is centered in the middle part of the eye.
Other causes are systemic, meaning they can affect multiple parts of the body:
Giant cell arteritis (GCA) – a form of vasculitis that mostly impacts arteries in the scalp and head. The first symptoms are typically headache, tenderness of the side of the head, tiredness and claudication (the jaws “locking up”). This condition can cause rapid blindness. GCA can also cause damage to the aorta — the largest artery in the body — as well as the heart.
Takayasu arteritis – an inflammatory condition that targets medium and large arteries. It is also called pulseless disease.
Polyarteritis nodosa – an inflammatory disease in which immune cells attack arteries. The cause of this disease is unknown.
Granulomatosis with polyangiitis – a rare inflammatory condition that impacts tissues throughout the body. It is largely centered around the respiratory tract and the kidneys. This condition was formerly called Wegener’s.
Secondary retinal vasculitis
Like primary RV, some causes of secondary RV are local to the eye:
Ocular sarcoidosis – a chronic disorder that can impact any part of the eye. Small groups of white blood cells (granulomas) form around affected tissue. This type of RV can be associated with fluid deposits (called “candle wax drippings”) just outside of the blood vessels.
Birdshot chorioretinopathy – a chronic form of uveitis. It creates lesions (areas of damage) in the inside back part of the eye (the fundus). It can also cause swelling in this area (cystoid macular edema) and the growth of new blood vessels (choroidal neovascularization) that can both cause severe vision loss.
Necrotic herpetic retinopathies – a group of conditions that damage the retina. They are caused by a herpetic virus. These conditions warrant immediate medical attention. The first symptoms are floaters, sensitivity to light and loss of vision in one eye.
Toxoplasmic retinochoroiditis – an infectious condition that causes inflammation in the retina. It is caused by the parasite Toxoplasma gondii.
Diffuse unilateral subacute neuroretinitis (DUSN) – an infectious condition caused by parasitic nematodes (roundworms). It creates lesions and inflammation throughout the retina.
Endophthalmitis – an infectious condition that impacts the inner coating of the eye. In severe cases, it can lead to blindness. RV is a potential outcome of the intravitreal antibiotics that are sometimes prescribed to treat endophthalmitis.
Eales’ disease – an idiopathic inflammatory condition. It typically involves vascular blockages, inflammation of vascular coatings (periphlebitis) and retinal neovascularization.
Branch retinal artery occlusion (BRAO) – a somewhat common ocular disorder. It creates a blockage (occlusion) in one of the branches of the central retinal artery. It can lead to vision loss.
Vogt-Koyanagi-Harada syndrome – a rare ocular condition. Its main focus is the central nervous system, but it specifically impacts vision and hearing.
Sympathetic ophthalmia – a rare condition that results in uveitis. It typically develops in one eye after an eye injury or eye surgery of the other eye.
Systemic causes of secondary RV include:
Primary intraocular lymphoma – a rare form of cancer. It is related to primary central nervous system lymphoma, which causes cancerous cells to grow in the lymph tissue of the brain and spinal cord.
Behçet’s disease – a chronic disease that can cause vasculitis throughout the body. Its exact cause is unknown. However, it’s considered an autoinflammatory disease in which the less specialized part of the immune system (the “innate” part) attacks one’s own body.
Multiple sclerosis – a disease in which the immune system attacks tissues in the central nervous system. This includes the brain, spinal cord and optic nerves.
Systemic lupus erythematosus (SLE) – a disease that causes the immune system to attack tissue throughout the body. Besides RV and inflammations of the eye, SLE can damage many other parts of the body, especially the kidneys. SLE can cause a butterfly-shaped rash on the face (malar rash).
Spondyloarthritis – a group of conditions that cause pain, stiffness and inflammation in the spine and joints. People suffering from spondyloarthritis usually have the HLA B*27 immune blood marker.
Inflammatory bowel disease – conditions that cause chronic inflammation of the gastro-intestinal tract. These conditions include Crohn’s disease and ulcerative colitis.
Relapsing polychondritis – a rare disease that causes inflammation in the cartilage. Its main impact is on the ears, nose, joints, eyes and throat.
Tuberculosis – a germ-based condition passed through the air. It most commonly attacks the lungs but can also attack other areas, such as the kidneys, brain and spine.
Syphilis – a sexually transmitted infection that can cause permanent damage throughout the body.
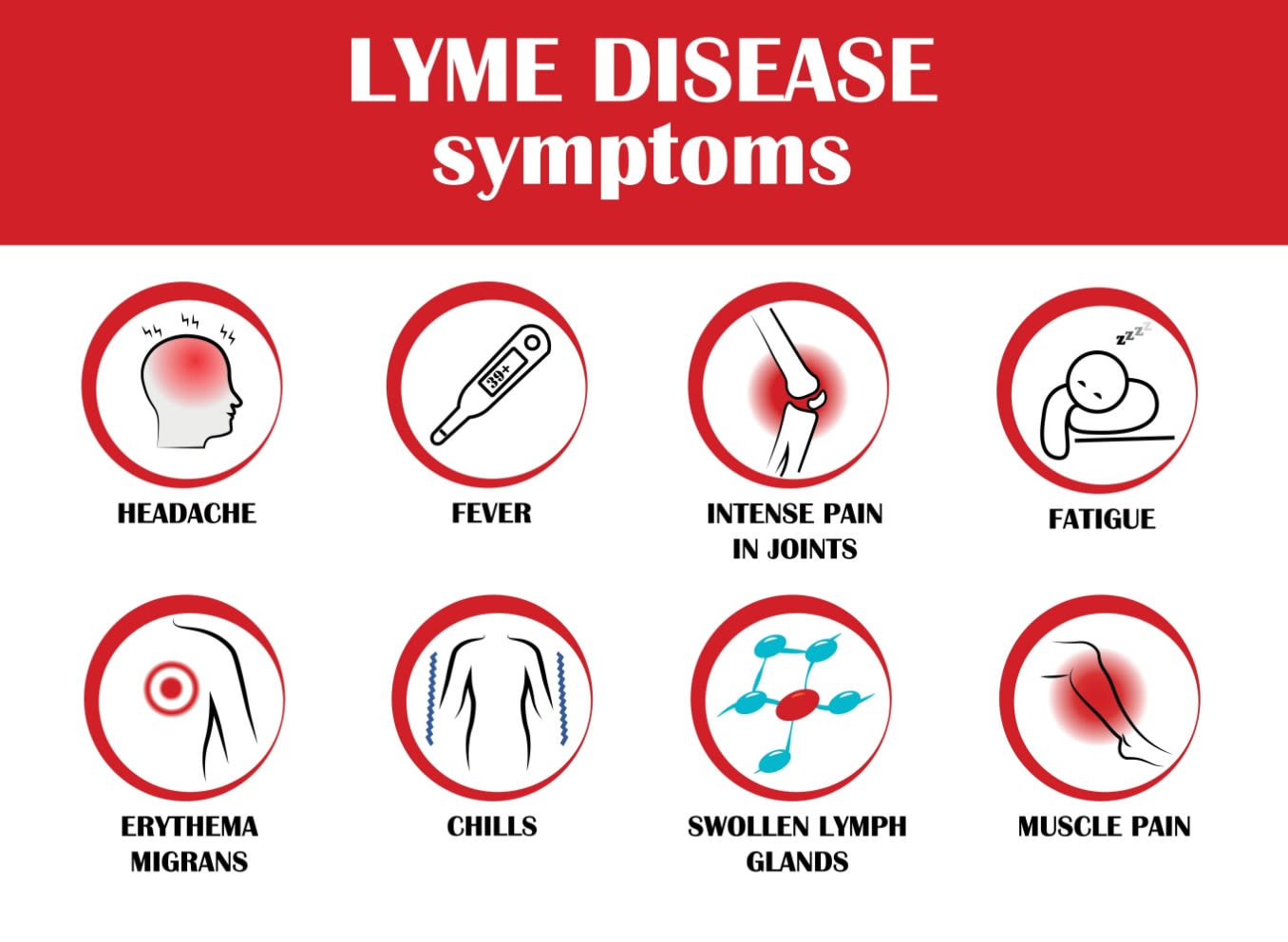
Lyme disease – a bacterial infection carried by deer ticks. It can cause rash, joint pain, nerve damage and many other issues throughout the body.
Viral infections (West Nile, HIV, cytomegalovirus) – infections caused by small germs (viruses). These germs use the body’s cells to duplicate themselves.
Cytomegalovirus – an infection caused by a herpetic virus. It is a common condition that is often asymptomatic. However, those with compromised immune systems and those who are pregnant are at higher risk for negative symptoms. It can cause fever, fatigue, rash, retinitis and other issues throughout the body.
Oculocerebral lymphoma – a rare form of cancer. It impacts the eyes and central nervous system.
Brucellosis – an infectious disease that more commonly appears in sheep, cattle, pigs and dogs. Humans can contract the bacteria by consuming unpasteurized dairy products and undercooked meat or through a penetration of the skin by the infected animal. It can cause a wide range of symptoms throughout the body, including ocular inflammation.
Sjögren’s syndrome – an autoimmune disorder characterized by dry mouth and eyes. It causes the immune system to attack glands that make moisture.
Rheumatoid arthritis – an autoimmune disorder that causes joint inflammation. It occurs when the immune system attacks the joints’ lining. While it usually impacts the hands, knees and ankles, it can also cause issues in the eyes, heart and lungs.
What are the signs and symptoms of retinal vasculitis?
Signs
The signs of RV reflect, and can help point a physician toward, the underlying cause of the condition.
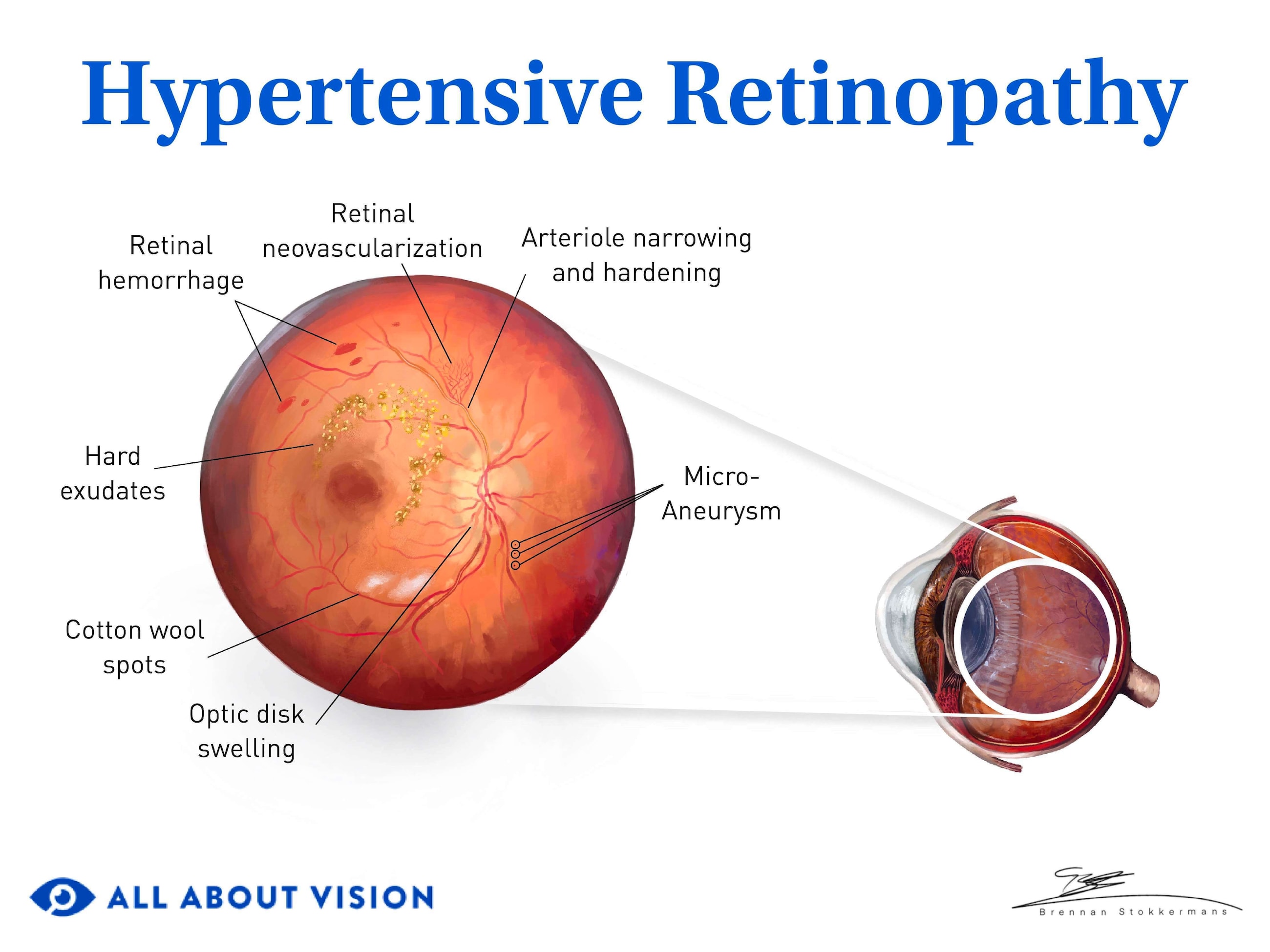
Perivascular sheathing
Perivascular sheathing is one of the most common signs of retinal vasculitis. It is a white cuff made up of inflammatory cells that appears around the blood vessels. It can indicate Eales’ disease, multiple sclerosis, sarcoidosis or tuberculosis.
Intraretinal infiltrates
Intraretinal infiltrates are bits of inflammatory cells and dead retinal tissue. They usually indicate an infection or an inflammatory condition. Intraretinal infiltrates can cause the retina to deteriorate and break, threatening sight. When they are close to the blood vessels, they are also called retinal “candle wax dripping.”
Cotton wool spots
Cotton wool spots are small areas of damage on the retina. They look like small, white-yellow clouds. They’re usually asymptomatic. Cotton wool spots may indicate SLE, polyarteritis nodosa or Churg-Strauss syndrome.
Retinal necrosis
Necrosis, or tissue death, may occur in the retina alongside the vasculitis. This is most common with infectious diseases. When retinal necrosis has just started, certain areas of the retina will appear bleached.
Frosted branch angiitis
Frosted branch angiitis can occur on its own. It can also be the result of an underlying, usually systemic, condition. It occurs when inflammatory cells coat retinal blood vessels, which then look like frosted tree branches. This inflammation can also cause retinal edema. It is most commonly associated with lymphoma and leukemia. However, it has also been linked to SLE, Crohn’s disease, toxoplasmosis and AIDS.
Retinal ischemia
Retinal ischemia happens when the retina’s blood supply is too low. This creates a lack of oxygen and can cause cells in the retina to die. Inflammation associated with vasculitis may cause an occlusion, or blockage, leading to ischemia. Retinal ischemia is often seen with SLE, tuberculosis and Behçet’s disease.
Symptoms
While retinal vasculitis can be asymptomatic, one of the main symptoms is loss of vision with no pain. Other symptoms vary in severity. Some cases of RV are mild with no impact on vision. More severe cases can cause pain and visual distortions. If you notice any of the following changes to your vision, it is important to see an eye doctor.
Floaters
Blind spots (scotoma)
Altered color vision
Visual distortions (metamorphopsia)
What are the stages of retinal vasculitis?
There are four stages of retinal vasculitis.
Inflammation stage: There is active inflammation of the blood vessels of the retina, choroid or uvea. The retina may also swell (retinal edema) and potentially burst (hemorrhage). In some cases, cysts can develop in the macula (central retina), leading to further swelling. This is called cystoid macular edema. There is also the chance of vascular occlusion that can decrease blood flow. Determining the cause of the RV during this stage is a priority.
Ischemic stage: Vascular occlusion may cause blood vessels to grow thin and white (sclerosed) or to become twisted (tortuous). There is often a lack of blood flow to the retinal tissue, called capillary nonperfusion (CNP).
Neovascularization stage: Neovascularization, the formation of new blood vessels, occurs in this stage. These new blood vessels typically form in areas they shouldn’t. They can also leak and cause inflammation and scarring. This can lead to vision loss. There is often blood in the vitreous — the clear, gel-like material in the middle of the eye — during this stage. This is called vitreous hemorrhage.
Complications stage: The damage at this stage is irreversible. This includes vitreous hemorrhage, retinal detachment and retinal scarring (epiretinal membrane). Neovascular glaucoma may develop. This means the newly developed blood vessels are blocking fluid from leaving the eyeball. This can cause the pressure in the eye to go up, resulting in damage to the optic nerve.
How is retinal vasculitis diagnosed?
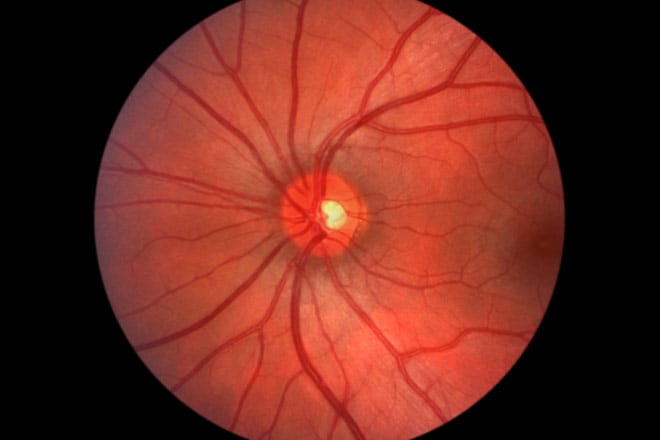
Retinal vasculitis is typically diagnosed by an eye doctor. The doctor will likely use both a slit lamp and indirect ophthalmoscopy for a full view of the eye.
A slit-lamp exam involves a microscope with a light attached to it that is used to view the front and inside of the eye. The patient’s pupils will be dilated to allow the physician to look at different layers of the eye. Indirect ophthalmoscopy is done with a device that attaches to the physician’s head. This exam gives the physician the ability to examine the back of the eye (the fundus).
They may also perform a scleral indentation as part of the indirect ophthalmoscopy. This means they will create a temporary indentation in the wall of the eye. This allows the physician to get a better view of the peripheral retina.
Fluorescein angiography is an imaging test that is often used to diagnose and monitor RV. To perform this test, the physician will inject dye (fluorescein) into a patient’s vein. As the dye moves through the eye’s blood vessels, a device will photograph it. This helps the physician see if there is appropriate blood flow to the eye.
If the underlying cause of the RV has not been diagnosed, other tests may be ordered. Blood tests, CT and MRI scans, chest X-rays and tissue samples may be taken. Determining any associated conditions is necessary for formulating a treatment plan.
There is no correlation between retinal vasculitis and age, gender, race or ethnicity. Because of this, it is important to report any sudden changes to your vision.
How is retinal vasculitis treated?
The underlying cause of retinal vasculitis will influence its treatment. For non-infectious RV, steroids and other immunosuppressants will likely be prescribed to decrease inflammation. When there is an infectious cause, certain antibiotics may be used.
RV can also lead to complications that require treatment, depending on its severity. Prescription eye drops can help with inflammation at the front of the eye. When new, abnormal blood vessels have grown in the iris or retina, these will need to be treated as well.
Other medications may be needed in addition to steroids to treat severe inflammation. These include:
Mycophenolate mofetil
Cyclophosphamide
Methotrexate
Adalimumab
Infliximab
Rituximab
While RV can be detected by any eye care provider, further testing and treatment generally requires a uveitis specialist. These doctors specialize in the treatment of eye conditions caused by inflammation or infections in the eye. If they identify an underlying condition, they will work with other specialists to create a treatment plan.
When should you see a doctor?
It is important to maintain regular eye exams if you have any of the listed underlying conditions. This can help your physician catch retinal vasculitis early. If you notice any sudden changes to your vision, such as blurriness, floaters, flashes or pain, seek immediate medical attention.