Contact an eye doctor immediately if you're experiencing a rapid onset of blurriness or loss of vision. A vitreous hemorrhage can quickly escalate into a very serious situation.
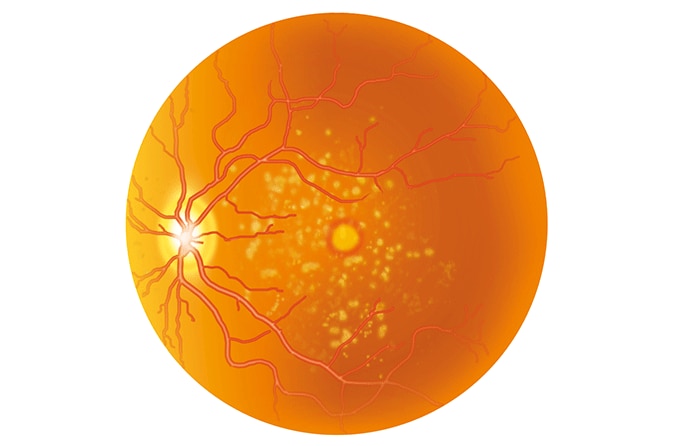
A vitreous hemorrhage occurs when blood from ruptured blood vessels leaks into the vitreous humor, the clear gel-like fluid of the eyeball. It has an incidence of 7 cases per 100,000 people each year in the U.S.
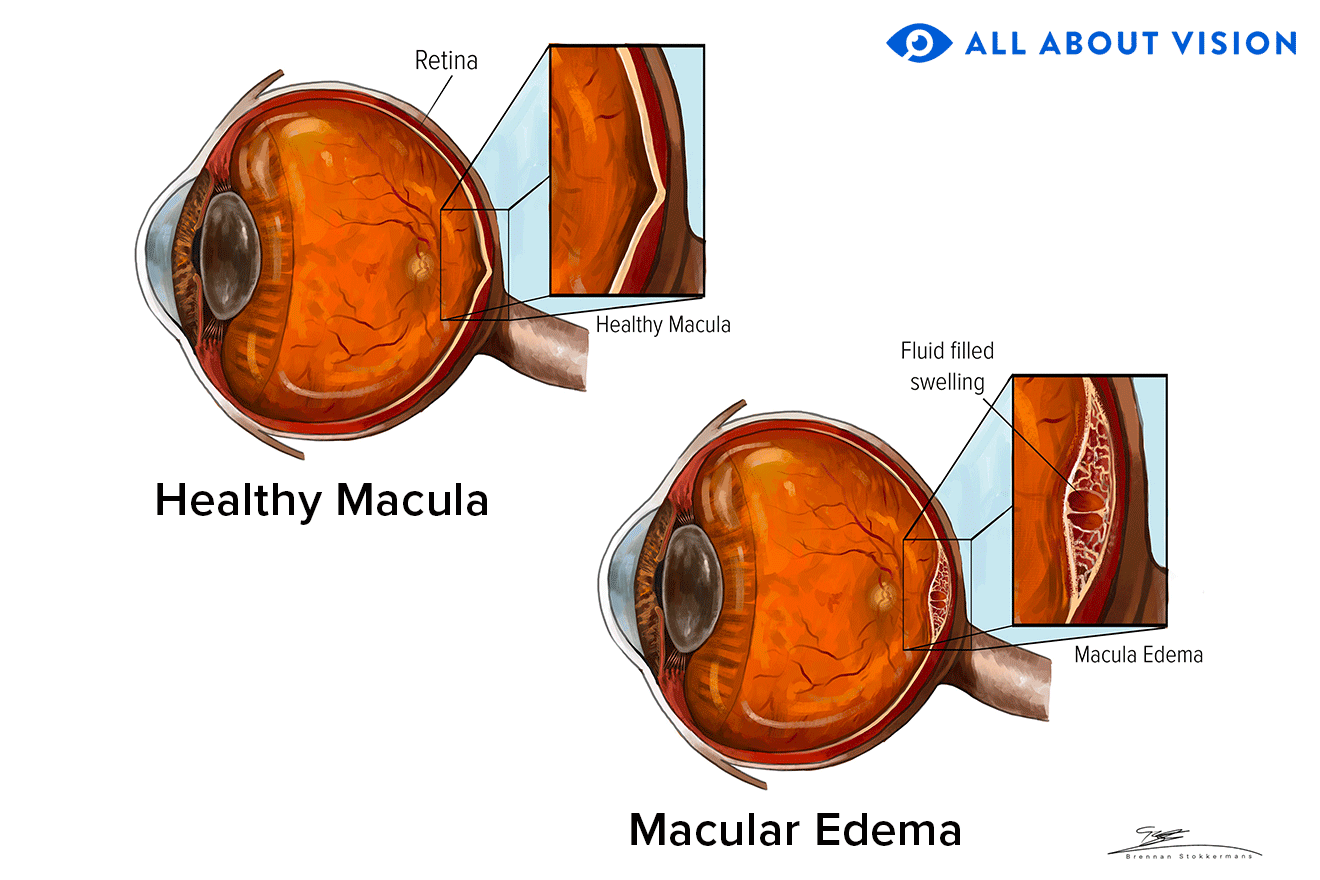
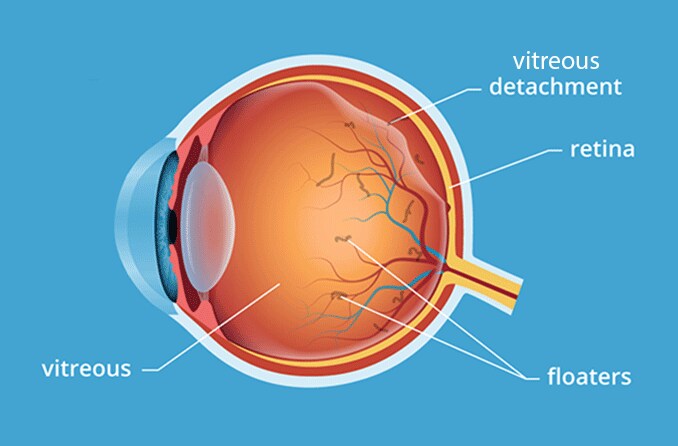
In the eyeball, vitreous humor (or just “vitreous”) is located in the vitreous chamber, the cavity between the lens (at the front) and the retina (at the back). This chamber makes up 80% of the eyeball and holds about 4 milliliters (or almost 1 teaspoon) of vitreous. This thick fluid plays very important roles in the eyeball: It maintains the eyeball’s spherical shape, keeps the retina in place and helps transfer light to the retina so you can process images.
When a vitreous hemorrhage takes place, you may suddenly see black spots or light flashes (photopsia). You may also experience blurriness, cloudiness or loss of sight. What's happening is the blood from ruptured blood vessels around the vitreous is entering the vitreous, getting suspended and obstructing the path of light to the retina.
If left untreated, a vitreous hemorrhage can threaten your visual acuity and lead to very serious complications, such as vitreous detachment, retinal detachment, optic nerve damage or ghost cell glaucoma.
Vitreous hemorrhage treatment
Once blood from ruptured vessels gets in the vitreous, it can clear on its own, be treated by trained eye specialists or be removed by surgery (vitrectomy).
Some treatments for a vitreous hemorrhage include:
Wait and see – This course of action may be advised for mild hemorrhages in which the bleeding stops and the blood gets reabsorbed by the body. Reabsorption occurs at a rate of 1% per day and may take two to three months to completely clear. Your eye doctor may suggest you sleep at a 45-degree angle and monitor all signs and symptoms in case the bleeding intensifies.
Laser photocoagulation – This treatment uses a hot laser beam to seal or destroy blood vessels under the retina that are leaking. The eye doctor will dilate your pupils with drops and then use the laser to do microscopic burns on affected areas, essentially cauterizing the ruptured blood vessels.
Anti-vascular endothelial growth factor (VEGF) medicine – This drug helps to stop the growth of abnormal blood vessels that rupture under the retina. The eye doctor will numb your eye with drops and then quickly inject an anti-VEGF drug into the vitreous. You may need one injection or several.
Cryotherapy – This procedure treats leaking retinal blood vessels by freezing eye layers and sealing the retina against the eye. The eye doctor will numb the area and then place a very cold probe on the white part of the eye ( sclera ).
Vitrectomy – Surgery may be needed after a vitreous hemorrhage when the body doesn't absorb the blood or the situation doesn't improve. The eye surgeon will drain the vitreous and replace it with a substitute since vitreous cannot regenerate on its own.
Vitreous hemorrhage causes
Common causes of a vitreous hemorrhage include:
Trauma or eye injury – Trauma to the eye from a direct impact by a blunt object or a puncture by a sharp object can cause blood vessels around the vitreous to be stressed, rupture and then leak into the vitreous. These traumatic injuries make up the majority of all cases of vitreous hemorrhages in people ages 40 years and under.
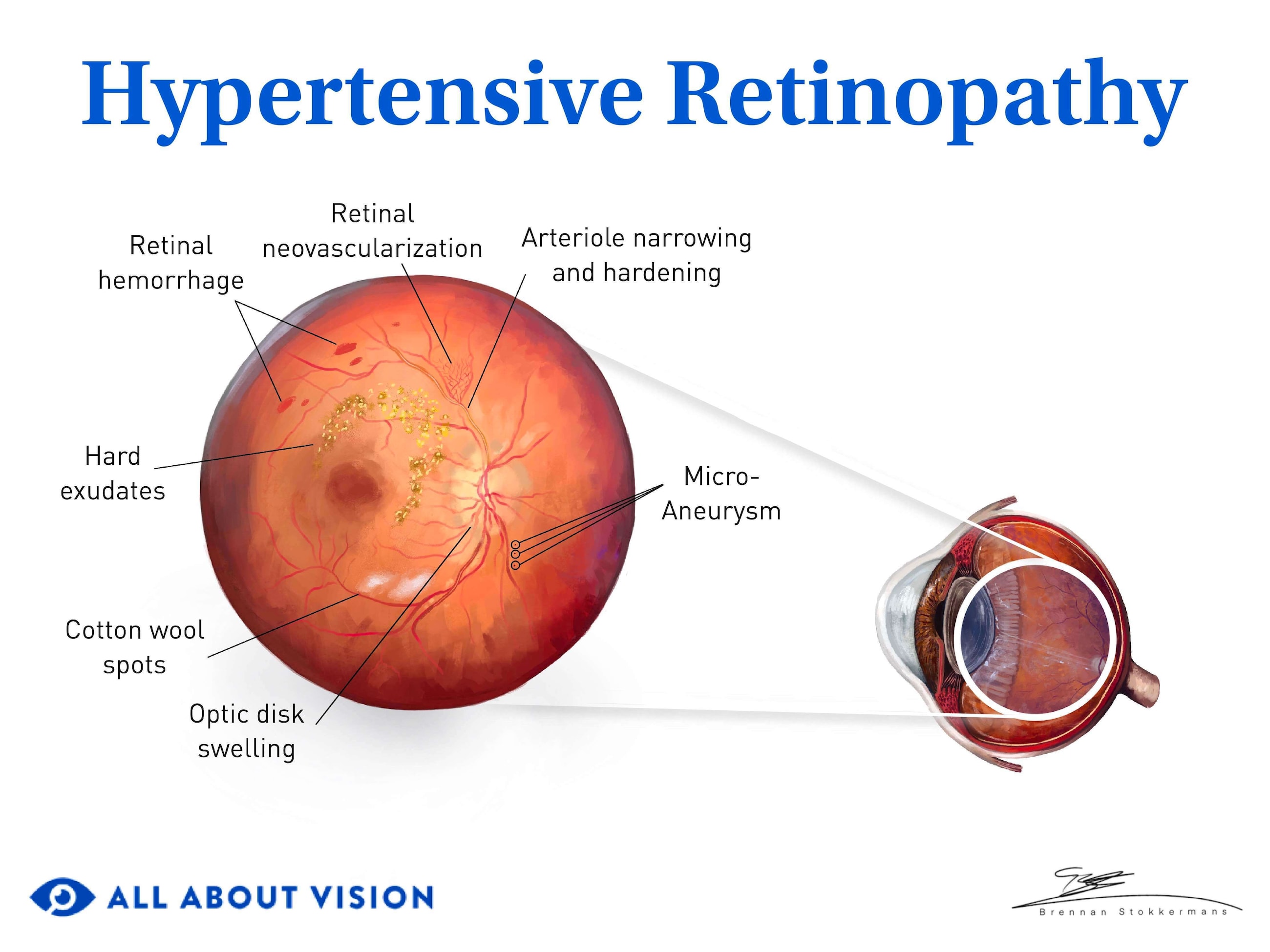
Proliferative diabetic retinopathy (PDR) – PDR is a common cause of vitreous hemorrhages in adults with diabetes, accounting for 31-54% of cases . It involves the formation of new blood vessels (neovascularization) that form in the retina. The vessels become prone to spontaneous rupturing and bleeding into the vitreous adjacent to the retina (posterior vitreous).
Posterior vitreous detachment (PVD) – A PVD can occur as part of the natural aging process of the eye. Over time, the posterior vitreous undergoes changes such as shrinking (vitreous syneresis). A hemorrhage can happen when the vitreous suddenly separates from the blood vessels that surround it (4-12% of cases) or when it suddenly pulls away from and tears the retina (11-44% of cases).
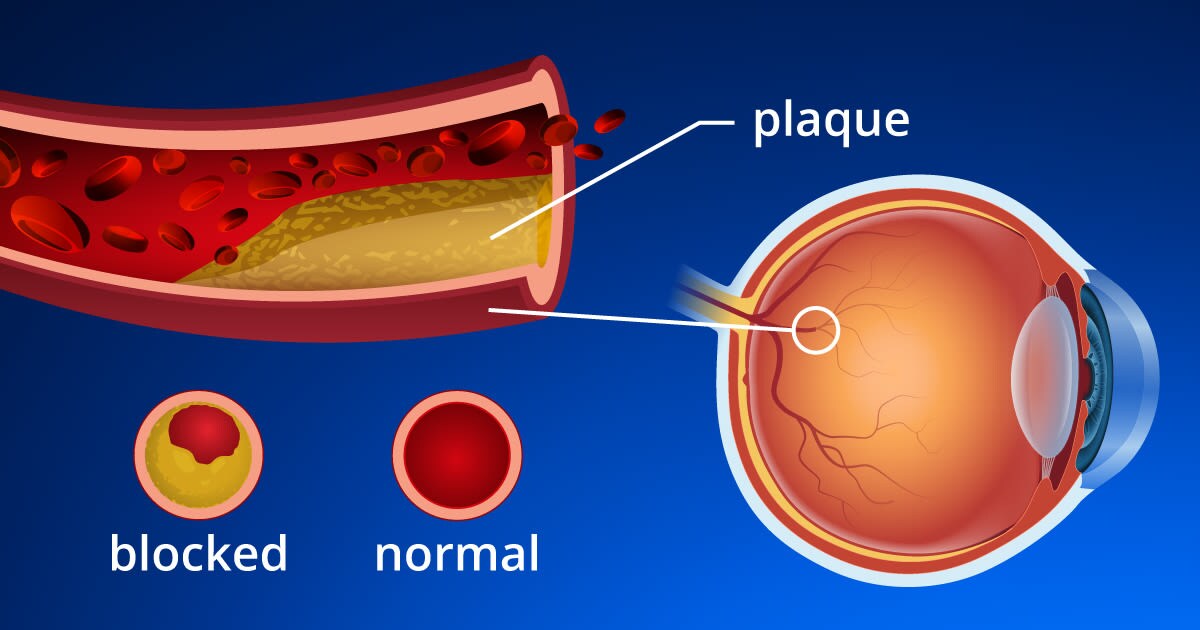
Retinal vein occlusion (RVO) – RVO involves the blocking of the retinal veins, which causes blood vessels to bleed into the vitreous. It also may cause abnormal blood vessels to form and then bleed into the vitreous. RVO is responsible for 4-16% of cases.
Less common causes of vitreous hemorrhages, in which blood enters the vitreous from a nearby source, include Terson syndrome, sickle cell retinopathy, eye tumors, retinal arterial macroaneurysm and age-related macular degeneration .
Vitreous hemorrhage symptoms and signs
The following are signs and symptoms of a vitreous hemorrhage:
Floaters like dots or specks in your field of vision
Lines or cobwebs
Flashes of light or dark streaks
Haziness, cloudiness or blurriness
Red hues
Blind spots ( scotoma )
Complete loss of vision
If you have a sudden onset of any of the above, contact an eye doctor as soon as possible for a comprehensive eye exam.
Vitreous hemorrhage surgery
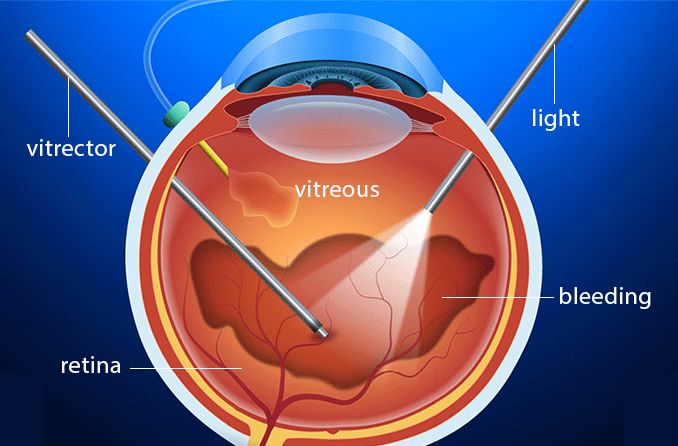
A vitrectomy corrects vitreous hemorrhages by removing a part of or the entire vitreous.
If the hemorrhage is mild, surgery may not be necessary. If the hemorrhage is severe, immediate surgery may be necessary as it may indicate an urgent situation such as a retinal detachment.
The eye surgeon makes tiny incisions and inserts instruments that assist in the drainage of part or all of the vitreous. Then, the vitreous is replaced with a substitute like saline to ensure the retina remains in its correct position in the eye. The incisions are closed with sutures or seal on their own.
During a vitrectomy, the surgeon may perform other procedures — repairing a retinal tear or macular hole or reattaching the retina — if needed.
When to see an eye doctor about a vitreous hemorrhage
Early detection by an eye doctor is imperative as a vitreous hemorrhage can worsen and cause serious issues.
During an eye exam, you may have one or more of the following tests to check the health of the eye as well as locate the source of the vitreous hemorrhage:
Slit lamp – After your eyes are dilated, your doctor will look into this instrument for a view into the vitreous.
Ocular ultrasound – A probe is placed over your closed eye and uses sound waves to look inside the eye. This procedure is especially useful for viewing the retina if blood is dense in the vitreous.
Optical coherence tomography (OCT) – This technology is used to take cross-sectional images of your eye’s layers using light waves. The OCT scans your dilated eyes, looking for signs of hemorrhages.
Fundus angiogram – A fluorescent dye is injected into your bloodstream so photos can be taken that show how the blood flows through blood vessels and to identify leaking or damage.
Contact an eye doctor near you to schedule an appointment if you're experiencing any signs or symptoms outlined here.