What is a cornea transplant (keratoplasty)?
A cornea transplant is when part or all of a damaged cornea is replaced with a healthy donor cornea. The cornea is the clear, dome-shaped “window” that covers your iris (the colored portion of your eye) and pupil that helps light focus inside your eye.
The medical name for a cornea transplant is keratoplasty (KAIR-uh-toe-plas-tee). You might also hear it called a corneal transplant or corneal graft.
Certain disorders, injuries and other things can permanently change the cornea in a harmful way. Light has to pass through the cornea before you can see it, so scarring or other changes can impair your vision. This may also be painful since the cornea is extremely sensitive.
A cornea transplant can help restore your vision, relieve discomfort and improve your quality of life.
Why would someone need a cornea transplant?
Ophthalmologists recommend corneal transplants for many reasons. They often involve at least one of these categories:
- Eye conditions that damage or inflame the cornea
- Eye infections
- Eye injuries
- Complications from another eye surgery
Common eye conditions that require surgery
Some common reasons why people need corneal transplants are:
- Fuchs’ dystrophy – The cornea swells and impairs vision as it gets worse. Small blisters can form on the cornea and burst.
- Keratoconus – The cornea gets thinner and changes shape over time. It develops into a more pointed cone shape instead of a round one.
- Pseudophakic bullous keratopathy (PBK) – Cornea swelling that can happen months or years after cataract surgery. It can lead to worsening vision and other vision changes. Advanced PBK can be painful.
- Corneal scarring – Damage caused by eye infections, injuries and other conditions, such as the ones listed above. Scarring can impair vision. In severe cases, it can lead to blindness in the affected eye.
- Previous corneal transplants – A failed transplant may require another transplant if it can’t be treated differently.
Types of cornea transplants
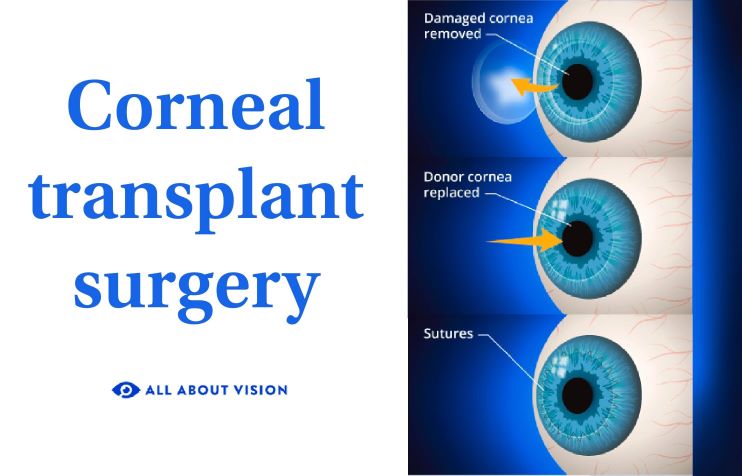
All corneal transplants involve removing damaged tissue from your cornea and replacing it with healthy cornea tissue from a deceased human organ donor.
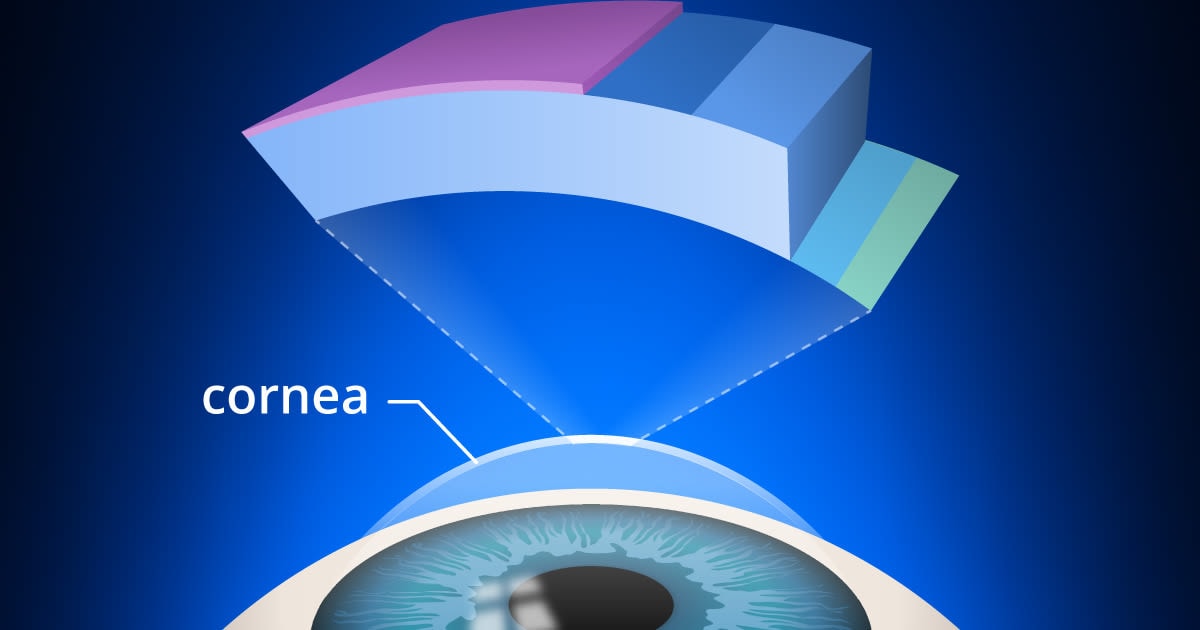
To understand the different types of transplants, it helps to learn about these five layers of the cornea:
- Epithelium – The sensitive outer layer that can heal itself
- Bowman’s layer – A tough inner layer that helps the cornea keep its shape
- Stroma – The strong middle layer that’s thicker than all other layers combined
- Descemet’s membrane – A thin inner layer that helps protect the inside of the eye
- Endothelium – The innermost layer that keeps the cornea clear

Corneal transplants usually aren’t used for problems that only affect the top two layers. Most of the time, at least one of the three lower layers is damaged, too. Some eye problems only affect the inner layers.
A keratoplasty can be categorized into two main categories: full-thickness or partial-thickness. Each category targets different layers of the cornea.
Full-thickness cornea transplant
A full-thickness corneal transplant is when all five layers of the cornea are removed and replaced with a healthy donor cornea.
There’s only one type of full-thickness transplant: penetrating keratoplasty (PK). It’s used when the entire width of the cornea is damaged, not just part of it.
While all of the cornea’s layers are removed during a full-thickness transplant, it doesn’t mean the surgeon removes your entire cornea. They only replace a portion of the cornea toward the center.
Partial-thickness cornea transplant
A partial-thickness corneal transplant is when only specific layers of the cornea are removed and replaced. The medical term is lamellar keratoplasty.
There are many different types of partial transplants. The eye surgeon’s choice depends on which parts of the cornea are damaged and other factors.
Overall, these grafts tend to heal more quickly with a lower risk of certain complications.
Endothelial keratoplasty (EK)
These transplants involve the back layers of the cornea. In particular, the endothelium (the deepest layer) is damaged and needs to be replaced.
Two of the most used corneal transplants are:
- Descemet’s stripping endothelial keratoplasty (DSEK) – Replaces the bottom two layers (endothelium and Descemet’s membrane) along with part of the middle layer (stroma). Descemet’s stripping automated endothelial keratoplasty (DSAEK) is a common variation of DSEK.
- Descemet’s membrane endothelial keratoplasty (DMEK) – Only the bottom two layers are replaced; the middle layer is not.
Anterior lamellar keratoplasty (ALK)
These grafts involve the cornea’s front (anterior) layers and the stroma in the middle.
The most common type of anterior transplant is deep anterior lamellar keratoplasty (DALK). During DALK, the eye surgeon removes the top three layers from your cornea but leaves the two lower layers in place. Sometimes, they do not remove all of the middle layer and leave a small part intact.
The surgery process
Transplants are performed by an ophthalmologist (a medical eye doctor who can perform surgery). Most surgeries will generally follow this process:
Before surgery
Your eye doctor will gather some information to see if you’re a good candidate for a corneal transplant. You can expect them to:
- Do a complete eye exam – A group of eye tests that help your eye doctor check your cornea, vision and overall eye health.
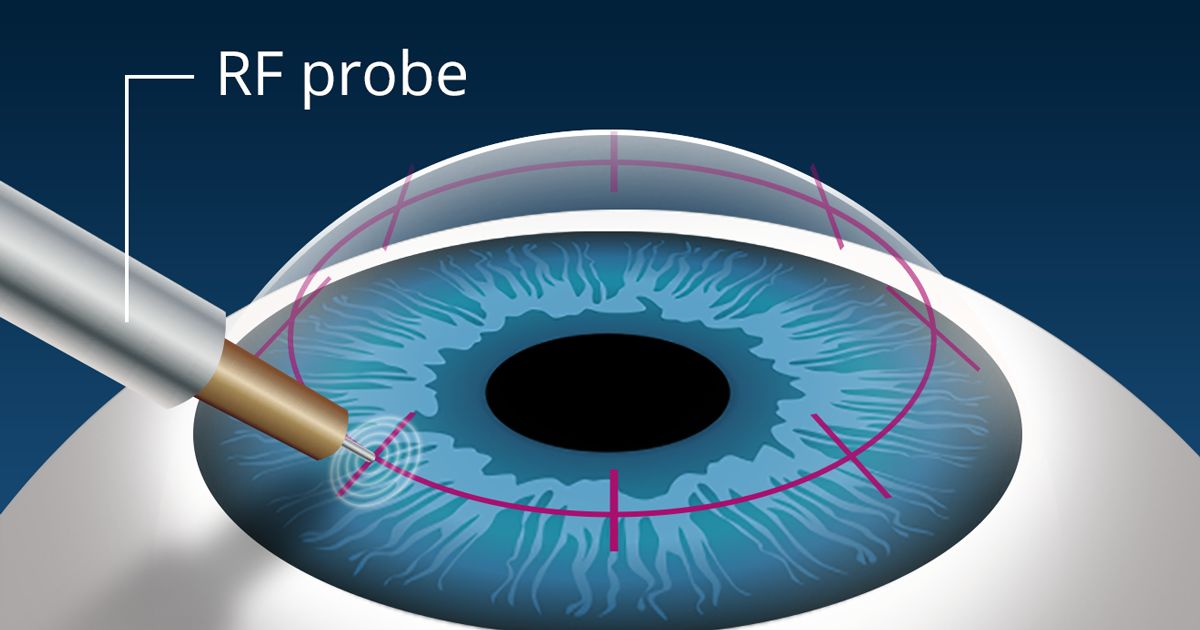
- Examine and measure your cornea – Specialized tests that help the doctor look for cornea changes and measure its exact thickness. This can involve tests like corneal topography, corneal pachymetry, optical coherence tomography (OCT) and others.
- Discuss your medical history and overall health – This information helps your eye doctor decide if your body can handle the surgery. Your primary care physician or other health specialists may be involved in this step.
Once they have the information they need, your eye doctor will talk to you about corneal grafts and how one could help your eyes. They’ll tell you what you can expect during and after surgery, including the potential risks.
If you and your doctor decide to move forward with the transplant, you’ll schedule a surgery date. You may need to wait until a donor cornea is ready for you, but this usually doesn’t take very long in the U.S.
Before your procedure, the eye doctor may ask you to:
- Stop taking certain prescription or over-the-counter medicines.
- Stop eating or drinking at a certain time before surgery.
How the surgery works
Cornea transplant surgery typically takes around one to two hours, no matter what type of procedure you have. It’s an outpatient surgery, which means you’ll go home the same day.
Your surgeon will likely follow these steps:
- Numbing eye drops are placed in your eyes so you can’t feel any discomfort.
- You may get an injection that either makes you very relaxed (a sedative) or puts you to sleep completely (general anesthesia). If you receive the sedative, you’ll also get an injection to completely numb the eye area.
- Once the medicine is working, the surgeon will use a tool to hold your eyelid open.
- The surgeon carefully removes the damaged parts of your cornea.
- The surgeon puts a matching piece of the healthy donor cornea in its place. They may use tiny stitches or an air bubble to keep the transplant secure.
- A protective shield is placed over your eye to keep it safe after surgery.
Recovering from a corneal transplant
Your vision in the affected eyes will probably look blurry for a while after surgery. This is because your eye is healing and adjusting to the new cornea.
Your eyesight should start improving within the first two weeks of surgery, but it can take up to a year or longer for your vision to fully recover.
Other mild side effects like these should go away within two weeks of surgery:
- Eye redness
- Eye irritation or soreness
Call your eye surgeon if you aren’t sure about something or if any symptoms are severe or last longer than they should.
Your surgeon will tell you to use steroid and antibiotic eye drops for several months after surgery (sometimes longer). The medicine in these drops helps your body accept the new cornea tissue, reduces swelling and lowers the risk of infection.
Precautions
As your vision gets better, you’ll slowly be able to go back to your regular activities. But your surgeon will tell you to take certain precautions first.
It’s very important to follow these instructions so you can lower your risk of complications and heal more quickly:
- Don’t rub your eye or press on it in any way.
- Wear your eye shield (or glasses) as long as your eye doctor says you need to.
- Don’t go back to work until your doctor says it’s okay (usually around one to two weeks after surgery).
- Don’t drive until your doctor says it’s safe and your vision meets the legal requirements where you live.
- Avoid contact sports for at least a month. After that, you’ll need to wear protective goggles to protect your eye.
- Don’t get water in your eye or go swimming (even with goggles) for at least a month.
- Don’t wear eye makeup for a month or so.
These timeframes can vary based on your surgery and other factors. Check your take-home paperwork for details or ask your eye doctor if you’re not sure.
Follow-up appointments
Your eye surgeon will need to see you regularly, so they can monitor your transplanted cornea and treat any problems. It’s very important to not miss these appointments.
Your timeline may vary a little, but you can generally expect to follow a schedule like this for your follow-up appointments:
- One day
- One week
- Two weeks
- One month
- Three months
- Six months
- One year
Most patients will also need follow-up exams after the first year.
If stitches were used for your cornea graft, the surgeon may need to slowly take them out during your follow-up visits. They may not fully remove them for several months to a year or more, depending on which corneal graft you had and how well your eye is healing.
Vision after a corneal transplant
Your eyesight should get clearer within a week or two after surgery, but it takes longer to get full vision in that eye.
You’ll need to keep wearing prescription lenses or sunglasses during this period, but don’t wear contacts until your eye doctor says it’s okay.
In general, patients can expect to have good vision in this amount of time:
- Between two and six months after an endothelial keratoplasty (patients who have DMEK may heal more quickly)
- Between 18 months and two years (but sometimes less) after an anterior lamellar keratoplasty
- Between one and two years after a penetrating keratoplasty
Risks and possible problems
Some patients have complications after surgery. The risk can vary, depending on the patient and which type of cornea transplant they have.
Possible complications
When complications happen, some tend to happen sooner after surgery while others might happen later.
In the first week or two after surgery, some people experience:
- Bleeding
- Infection
- Corneal abrasion (scratch)
Other possible complications may develop later on. Some of them are:
- The eye disease that was treated comes back
- The surgery wound reopens
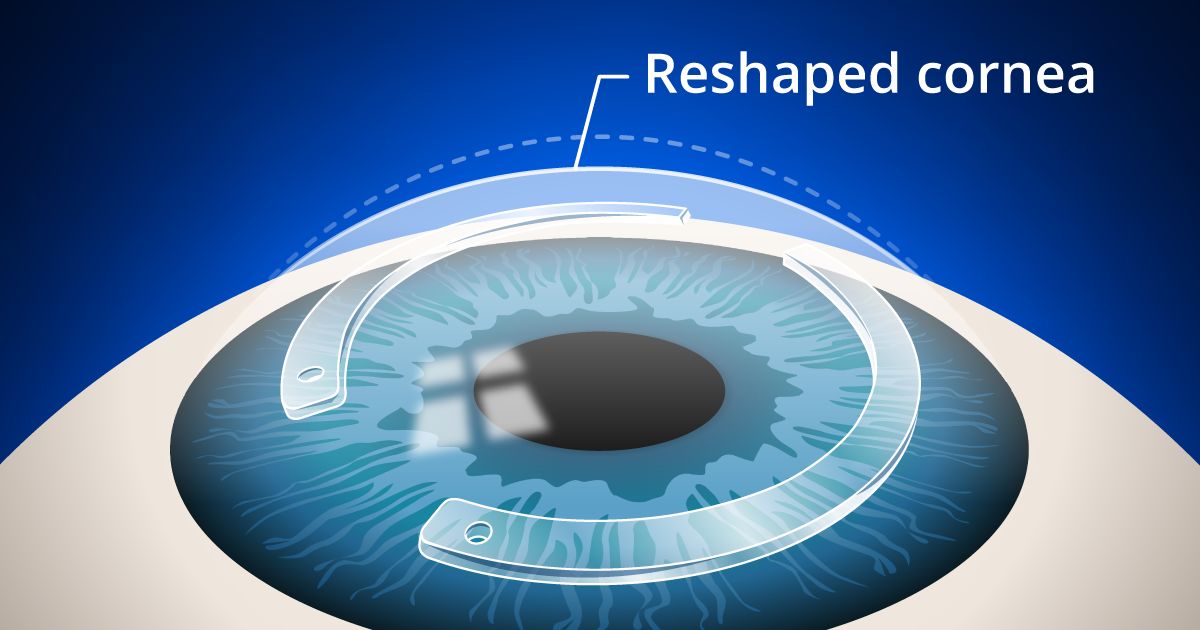
- Astigmatism (the shape of the cornea makes your vision blurry)
- Glaucoma (high fluid pressure inside your eye)
- Retinal detachment (the thin retina layer pulls away from the back wall of your eye)
- Macular edema (swelling at the center of the retina)
Cornea graft rejection
Like other kinds of transplants, there’s a risk that your body will reject the donated cornea and attack it.
This is called a graft rejection or transplant rejection. It’s more likely after a full-thickness keratoplasty (PK) and least likely after DMEK.
The symptoms of graft rejection can start as soon as 24 hours after surgery, but rejections can also happen weeks, months or even years later.
Fortunately, most rejections are mild and can be treated with steroid eye drops. Early treatment is critical.
Graft failure
In rare cases, a rejection is severe or lasts a long time and doesn’t respond to treatment. This is called a graft failure because the new cornea fails and gets cloudy. If this happens, another cornea transplant or other eye procedure will be needed.
If the grafts keep failing, your eye doctor may recommend an artificial cornea transplant (keratoprosthesis).
When to call your eye doctor
Most complications (including a transplant rejection) need to be treated quickly. Without treatment, these problems can get worse and permanently damage your new cornea tissue or other parts of your eye.
Don’t wait — tell your eye doctor right away if you have symptoms, like:
- Your eyes appear very red.
- You have a lot of eye pain.
- The transplanted cornea looks cloudy.
- Your vision looks cloudy.
- You have blurry vision that doesn’t go away.
- You experience severe light sensitivity.
- You notice new eye floaters or flashes of light in your vision.
- It looks like a dark curtain is moving across your view.