What is laser photocoagulation eye surgery?
Laser photocoagulation is a procedure that uses a laser to treat retinal conditions. It can slow down or prevent serious complications that can lead to vision loss. It is used to manage conditions such as diabetic retinopathy, macular edema, retinal vein occlusion and retinal holes or tears.
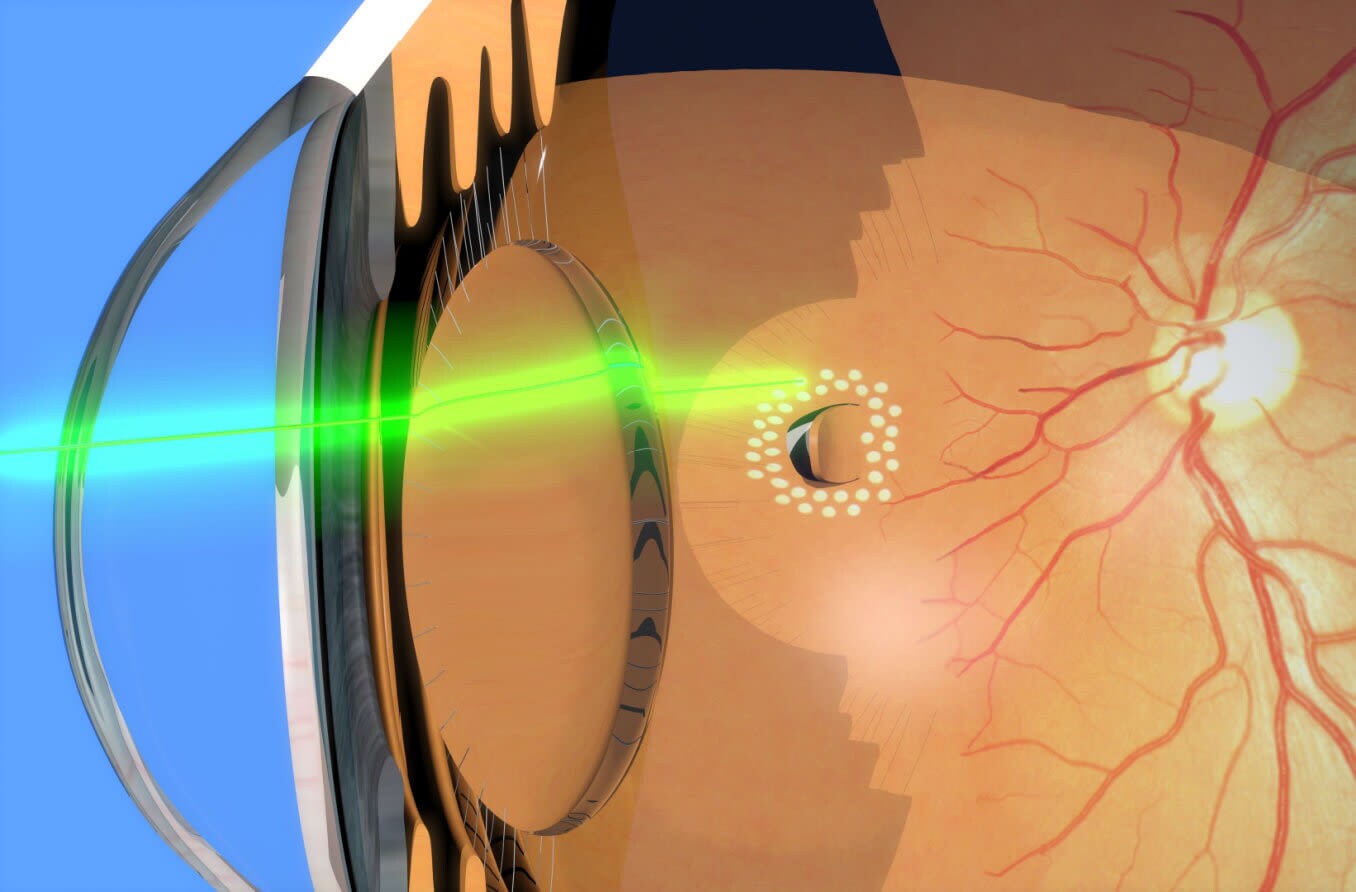
How laser photocoagulation works
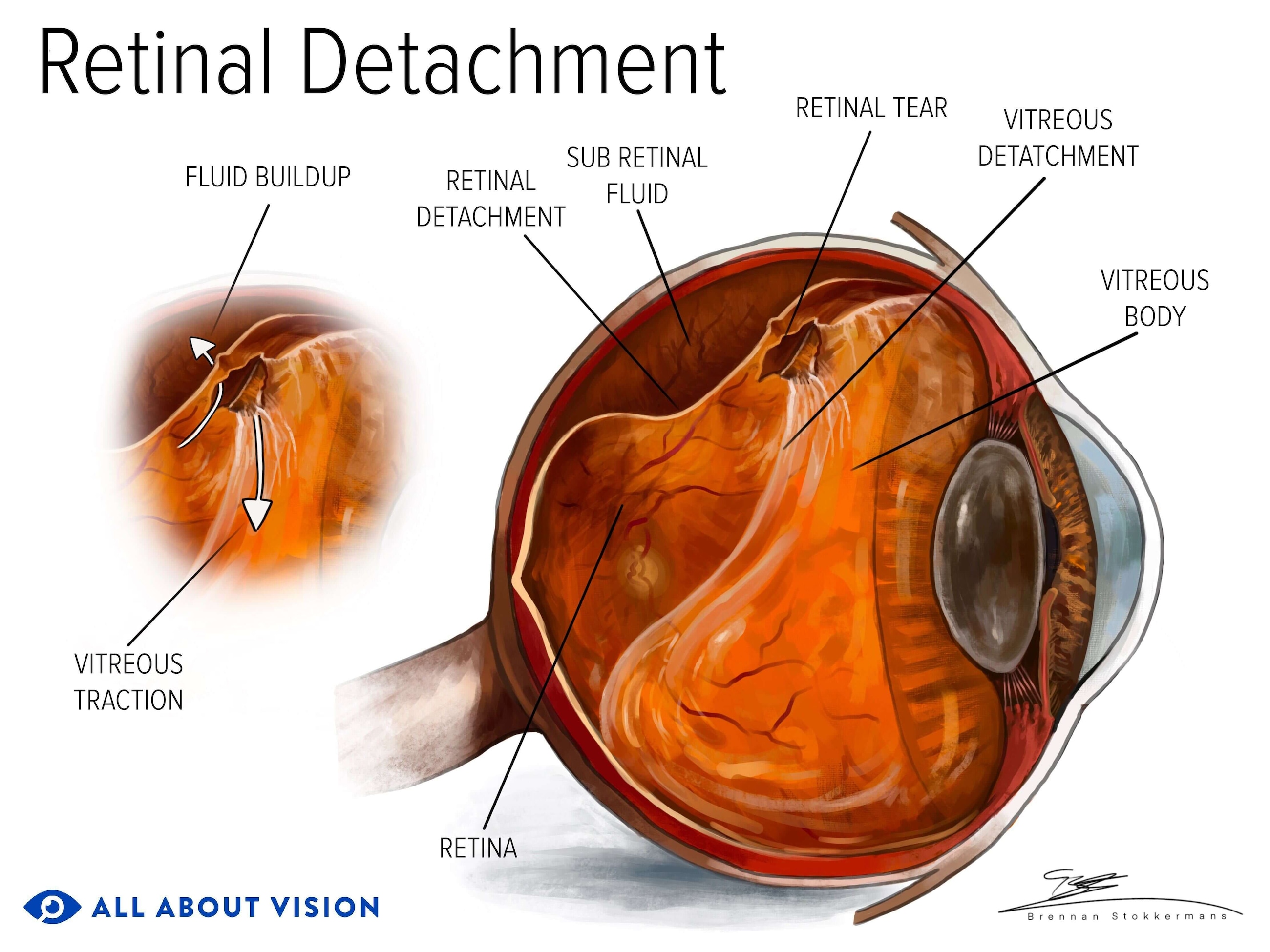
Laser photocoagulation uses a laser to generate heat and create a burn. This burn develops into scar tissue in a targeted area of the retina — the light-sensitive tissue in the back of the eye. Retinal photocoagulation uses different lasers than other laser eye surgeries, such as glaucoma surgery or refractive surgery, like LASIK.
The scars generated by the laser stabilize vision by sealing off abnormal and leaky blood vessels that develop in certain retinal diseases. Laser photocoagulation can also help treat complications, such as swelling in the retina, by decreasing fluid leakage. In some cases, the unhealthy retina is treated with lasers to preserve the healthy retina.
In addition, the burn created by laser photocoagulation can help to adhere or weld down a tear or hole in the retina, preventing it from becoming larger. This can also be done with small retinal detachments, walling them off, so they do not progress.
What to expect during the procedure
Laser photocoagulation is a minimally invasive outpatient procedure. It is usually performed at an ophthalmology office or clinic. The treatment is relatively painless and lasts less than half an hour.
Because the treatment is not invasive, you can return home shortly after the surgery. However, you should not drive home. Instead, arrange for someone to accompany you and drive you home.
In general, the steps of the procedure are as follows:
Explanation of the procedure by your eye doctor
Numbing and dilating eye drops placed in the eye
Chin positioned in chinrest and eyes looking ahead, or at a target
Placement of a focusing lens on the eye being treated
Laser treatment pulses on the targeted area of the retina
Eye drops to prevent inflammation placed in the eye
During the laser treatment, you may see light flashes or experience other mild sensations. But your eye doctor will ensure you are comfortable.
During the one or two-day recovery period after the procedure, you may experience slight discomfort or mild pain in the eye. You will have a follow-up appointment a few days after the procedure so your doctor can see how you are healing.
The number of sessions that are needed will depend on your eye condition and the severity of complications. An eye doctor will watch your progress to see how many sessions are needed. Follow-up appointments may be needed for weeks and months after the first session.
Depending on the condition being treated, most individuals may be able to resume their normal routine within a day or so. When a retinal hole or tear is being treated, an eye doctor may restrict activity for one or two weeks.
What conditions can be treated with the procedure?
Laser photocoagulation can be used to treat a wide array of conditions. In many cases, laser photocoagulation prevents the worsening of vision. In some instances, vision can improve afterward. This treatment may be performed in addition to other procedures, such as injected medication or other types of laser.
Diabetic retinopathy
People who have diabetes sometimes develop a complication in the back of the eye (retina) called diabetic retinopathy. This is because diabetes damages the blood vessels in the body. In the retina, diabetes causes the blood vessels to swell and become leaky.

In some cases, diabetes can also lead to neovascularization — the growth of new and abnormal blood vessels — in the retina. This advanced form of diabetic retinopathy is called proliferative diabetic retinopathy. It requires laser photocoagulation because the new vessels leak blood and fluid, damaging the retina and causing vision loss.
Typically, pan-retinal photocoagulation (PRP) is performed in cases of proliferative diabetic retinopathy. This procedure uses hundreds of laser spots to destroy the abnormal blood vessels growing in the outer retina to preserve the central retina and central vision. A slight loss of side vision may result. Several sessions are required for this treatment.
Macular edema
Certain conditions, including diabetes, can cause the area in the center part of the retina — the macula — to swell. The macula is responsible for our detailed, central vision. Swelling, or edema, in this area will result in decreased vision.
An eye doctor will perform focal laser therapy (FLT) to seal off the abnormal blood vessels in the central retina to help dry up the fluid causing the edema.
READ MORE: Diabetic retinopathy and diabetic macular edema
Retinal vein or artery occlusion
Retinal vein occlusions are treated with focal photocoagulation when macular edema is present. When a retinal vein or artery occlusion leads to neovascularization, pan-retinal photocoagulation is used to prevent further vision loss from complications.
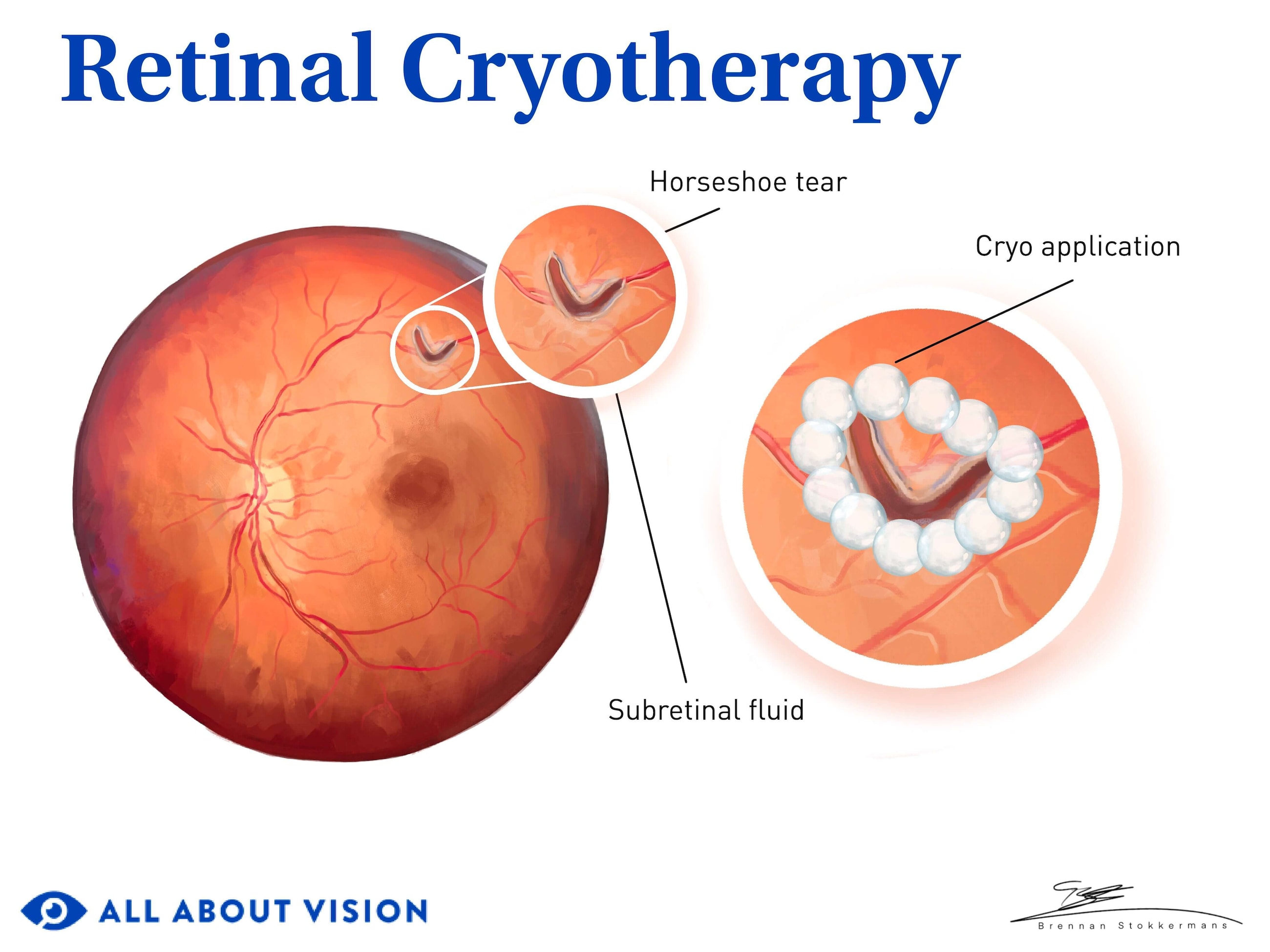
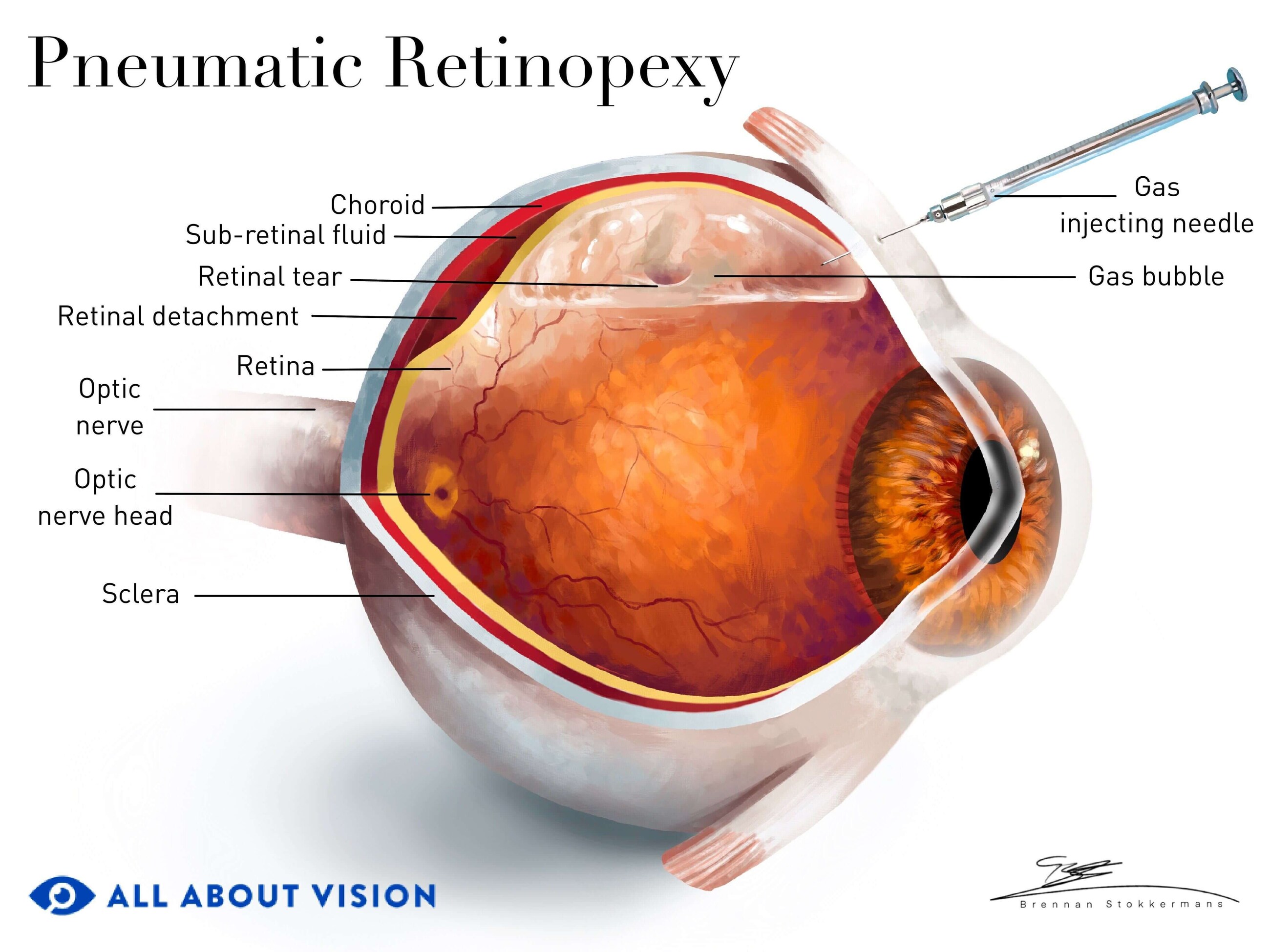
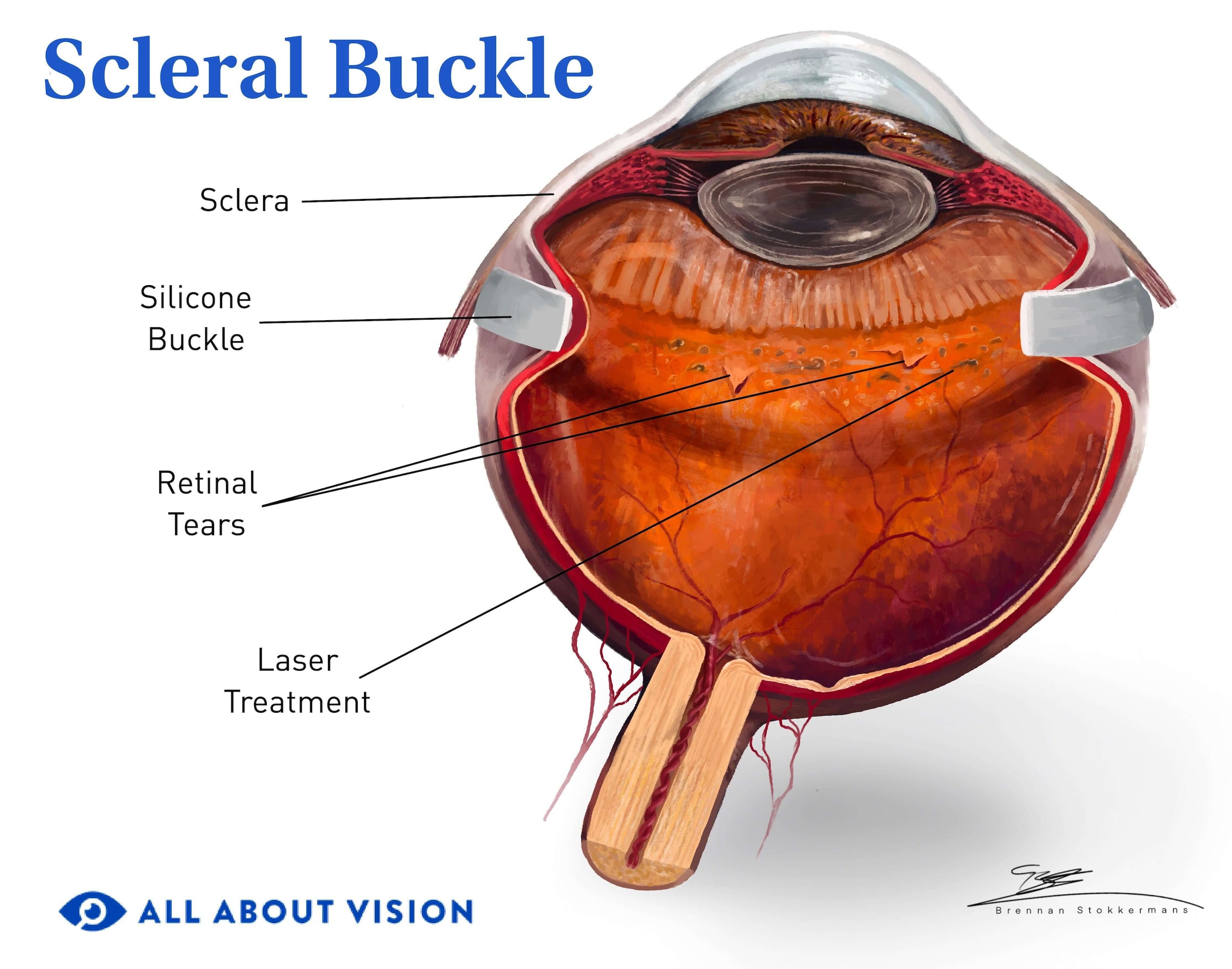
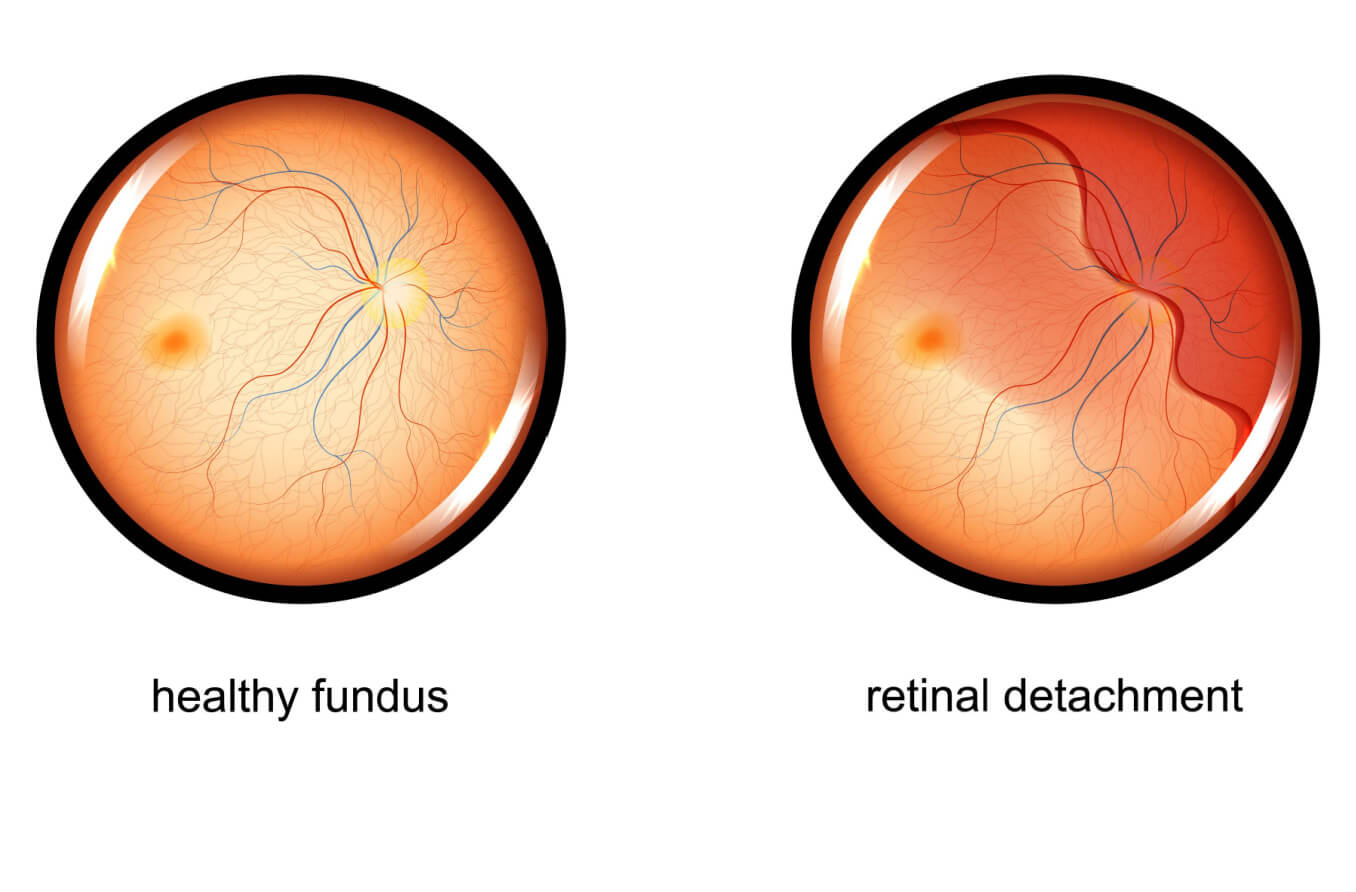
Retinal hole or tear
If the retina develops a hole, tear or detachment, a procedure called laser retinopexy can be performed to help repair the retina. This procedure creates a wall of scar tissue around the hole, tear or small detachment, welding it to the underlying tissue. This prevents it from progressing into a larger retinal detachment, which can lead to severe vision loss.
It can take one or two weeks for healing to occur, so your activity may be restricted during this time.
Choroidal neovascularization in wet macular degeneration and other conditions
Retinal photocoagulation is sometimes used to treat new blood vessel growth under the retina, known as choroidal neovascularization. These new blood vessels under the retina develop in wet macular degeneration as well as other conditions. But when the treatment area is near the center of vision, this procedure can cause a blind spot.
Due to this, other treatments, such as photodynamic therapy (PDT), are either preferred or used in combination. PDT uses a laser that is activated by an injected medicine. The laser does not cause a heat burn, so the central retina does not get damaged as it would with laser photocoagulation.
SEE RELATED: Toxocariasis and Lattice degeneration of the retina
What are the pros & cons of laser photocoagulation?
Laser photocoagulation has several pros and cons. It is generally low-risk, and side effects are typically not severe. The cons of this procedure depend on your treatment type and the condition that is being treated.

Some individuals may have a slight decrease in their central visual acuity. Side vision may be reduced in some cases. In addition, night vision and vision in low-light settings may be mildly reduced. Finally, some individuals report a decreased ability to focus up close.
It is common to feel nervous about the treatment. Retinal laser photocoagulation is a minimally invasive in-office procedure that can preserve eyesight. This procedure has been used for several decades with much success in preserving vision. It can save the remaining vision that may be lost if the retina is not treated. In some cases, vision may even improve because the procedure has reduced the amount of swelling in the retina.
If your eye doctor has recommended retinal laser photocoagulation, it is because the pros greatly outnumber the cons. If you have concerns regarding the procedure — such as its effect on your vision, complications or the cost of the procedure — speak with your eye doctor. They can answer questions regarding your specific condition.