What conditions do eye surgeries treat?
There are many different types of eye surgeries, treating a wide array of eye conditions. Some of these conditions include glaucoma, cataracts, retinal tears and detachments, wet AMD, diabetic retinopathy, and even nearsightedness and farsightedness.
In addition, eye surgeries address issues in the muscles around the eye or the cornea — the clear structure at the front of the eye. The cornea can lose its transparency and requires a transplant. Eye muscle surgery is sometimes necessary to align the eyes and reduce double vision.
Tumors can develop in and around the eye and may need to be surgically removed. Surgery can also be done around the eyes, such as to repair eyelids.
Cataract surgery
Most people are familiar with cataract surgery — the removal of the eye’s natural lens that has become cloudy with age and replacement with a clear artificial lens.
Procedure
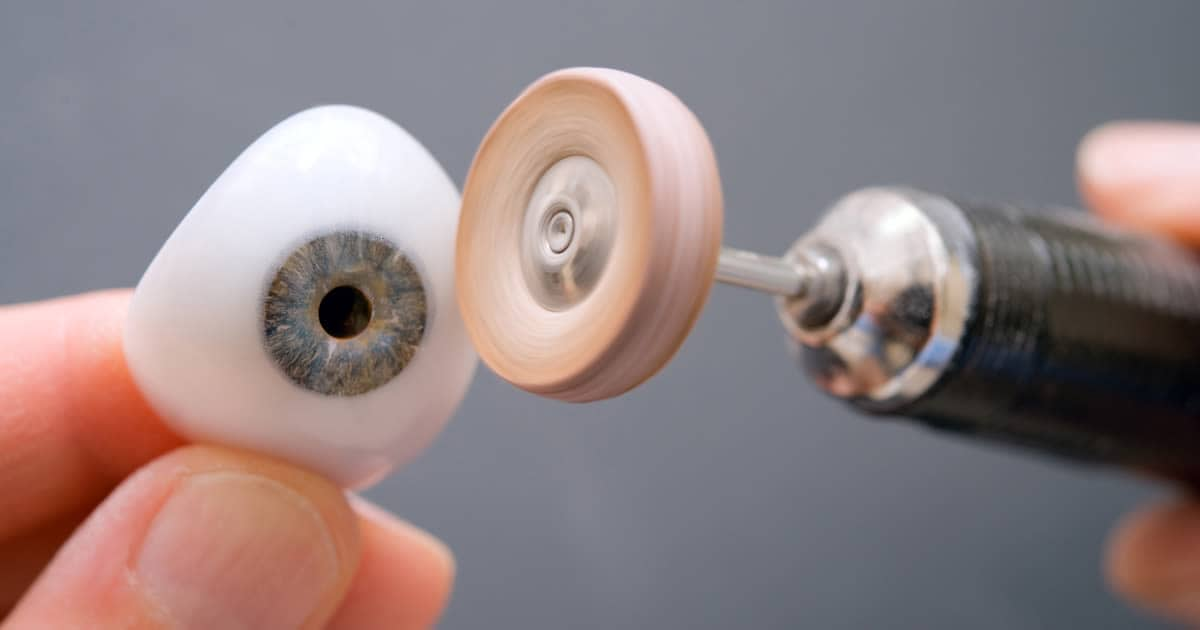
During cataract surgery, the surgeon removes the cloudy natural lens and replaces it with a clear artificial lens called an intraocular lens (IOL). The IOL is placed inside the lens capsule that held the natural lens. It is a common surgery and carries a low risk. The surgery takes about 15 minutes, and you will be able to go home that day.

The tiny, clear IOL replaces the natural lens inside your eye. [Image credit: By Frank C. Müller licensed under CC BY SA 3.0 ]
The standard IOL is monofocal — it corrects vision at one distance, usually far away. People with astigmatism may have prescriptions that standard IOLs cannot fully correct. A premium toric IOL may be needed to correct their astigmatism.
For those who desire to stop wearing reading glasses after cataract surgery, accommodating IOLs and multifocal IOLs are good options. These allow focus at distance, intermediate and near. These IOLs can end the need for reading glasses.
Conditions that require cataract surgery
There are different types of cataracts that can develop in the eye. Symptoms of cataracts include:
Decreased vision, with near vision worse than distance vision
Sensitivity to bright lights
Glare, especially from headlights when driving at night
Halos around lights
When the cataract begins to interfere with activities of daily life, cataract surgery is performed.
Nuclear cataract
A nuclear cataract is the most common type of cataract in the senior population. It is a clouding and hardening of the lens center, resulting in blur, glare and other changes in vision. It takes many years for nuclear cataracts to develop.
Cortical cataract
A cortical cataract is an opacity in the outer layer, or cortex, of the natural lens. It is more common in people with diabetes and hypertension.
Posterior subcapsular cataract
A posterior subcapsular cataract (PSC) is a fast-growing opacity in the rear of the natural lens. This cataract is most common in people who take steroids or have diabetes.
YAG laser capsulotomy for posterior capsular opacification (PCO)

A laser capsulotomy is a relatively simple, in-office procedure that takes only a few minutes. A laser beam is directed at the cloudy capsule behind the intraocular lens (IOL) and the energy from the laser vaporizes the tissue, restoring clear vision.
Although posterior capsular opacification is sometimes called a “ secondary cataract,” it is not a cataract. The IOL has not become cloudy. The back of the capsule in which the IOL is implanted has become cloudy. It is the most common complication of cataract surgery. About one in five people develop PCO within one year after cataract surgery. About one-third develop PCO after five years.
PCO usually develops slowly, much like a nuclear cataract. A procedure called YAG laser capsulotomy is performed to treat it. This outpatient procedure requires eye dilation but is generally quick and painless and does not require an incision. A laser beam is directed at the posterior part of the lens capsule, cutting away the cloudy tissue and restoring clear vision.
Glaucoma surgery

Glaucoma surgery is performed to lower the pressure inside the eye in people with glaucoma. When the pressure in the eye is too high, the risk of vision loss increases due to damage to the optic nerve, which sends signals from the eye to the brain. Glaucoma surgery cannot recover lost vision but can help prevent further vision loss.
A laser can be used to perform several types of in-office glaucoma surgeries, and only numbing drops are usually required. If medication and laser surgeries haven’t been effective, other types of glaucoma surgery that require an incision and local anesthetic may be necessary.
These are the most common laser glaucoma surgeries:
Argon laser trabeculoplasty (ALT)
This in-office procedure is typically performed on people with open-angle glaucoma who have high eye pressure because the fluid in the front of the eye — called aqueous humor— is not draining properly. This is the type that most people with glaucoma have. In general, the pressure increases slowly over time.
Selective laser trabeculoplasty (SLT)
This procedure is similar to ALT, but a cold laser is used instead of a thermal laser, reducing scar tissue and allowing it to be a repeatable procedure. It has gained popularity as the first line of treatment for people with open-angle glaucoma.
Procedure for ALT and SLT
After the eye is numbed, a special lens is placed in front of it, and a thermal laser is directed at the drainage meshwork. The laser makes drainage more effective, resulting in lowered eye pressure within the next few months.
This procedure only takes a few minutes and is generally painless, although you may notice some flashes of light while it is performed.
Laser peripheral iridotomy (LPI)
This in-office laser procedure is used to treat or prevent narrow-angle glaucoma. This type of glaucoma is much less common. It is due to a narrowing of the angle — the junction at which the iris and cornea meet — through which fluid flows out of the eye. This angle can close, resulting in a sudden increase in eye pressure.
Narrow-angle glaucoma requires a different type of surgery than open-angle glaucoma. In narrow-angle glaucoma, the meshwork drains properly, but the drainage area has narrowed or closed.
Procedure for LPI:
The procedure begins by placing an eye drop that makes the pupil smaller and an eye drop that numbs the eye. A special lens is placed in front of the eye, and the laser makes a small hole in the iris of the eye, allowing fluid to flow through it.
This procedure only takes a few minutes, is generally painless, and you may notice some flashes of light while it is performed.
Trabeculectomy
This filtration surgery requires an incision and is used to treat open-angle glaucoma. It is performed in a hospital when medication and laser surgery are ineffective. Typically, you are able to go home the same day as the surgery, although someone will need to drive you.
Procedure for trabeculectomy
The surgery lasts about one hour and involves creating an opening under the eyelid in the whites of the eye, the sclera, to allow excess fluid a new pathway to drain. The opening is covered by a thin tissue called the conjunctiva, creating a “bleb” on the sclera.
Glaucoma implant surgery and minimally invasive glaucoma surgery (MIGS) are newer procedures that also require an incision.
Refractive surgery
Refractive errors such as myopia, hyperopia and astigmatism can be corrected with refractive surgery. These vision surgeries are procedures that modify incoming light rays, so they are focused directly on the retina, providing clear vision.

In LASIK, a large opening is required to enable the excimer laser to reshape the underlying cornea.
LASIK
The most well-known refractive surgery is LASIK — laser in-situ keratomileusis. This procedure reshapes the tissue under the cornea’s surface by creating a flap and targeting it with a laser.
Wavefront-guided LASIK uses computer imaging technology to reduce some of the side effects of LASIK, such as decreased contrast sensitivity and poor night vision.
PRK
PRK, or photorefractive keratectomy, also reshapes the cornea but does not require a flap. The top layer of the cornea is removed so that the laser can reshape the cornea. The top layer then grows back over the next several days.
LASEK
Laser subepithelial keratomileusis is similar to PRK, but a flap is created and placed back after the laser treatment. Some experts believe that this provides a more comfortable experience and faster recovery.
EpiLasik
The cornea’s top layer is thinly separated and lifted to the side during the procedure for EpiLasik. The layer underneath is lasered similarly to PRK, and a soft contact lens is applied as a bandage to help the cornea heal over the next several days.
Conductive keratoplasty (CK)
This procedure corrects low amounts of farsightedness. A probe applies heat to the edges of the cornea, causing the tissue to shrink. The goal is to focus light on the retina instead of behind it.
Refractive lens exchange (clear lens extraction)
Refractive lens exchange is a similar procedure to cataract surgery. But, the eye’s clear natural lens is replaced with an artificial lens to correct a refractive error. The eye’s natural ability to focus up close is lost.
An IOL that allows some accommodation or focusing at multiple distances can be selected to compensate for this loss.
Phakic intraocular lenses (IOLs) / implantable contact lens (ICL)
A phakic IOL provides a refractive surgery option in cases of very high refractive error. The eye’s natural lens is not removed, but a phakic IOL is placed in front of it. This procedure retains the eye’s ability to focus up close.
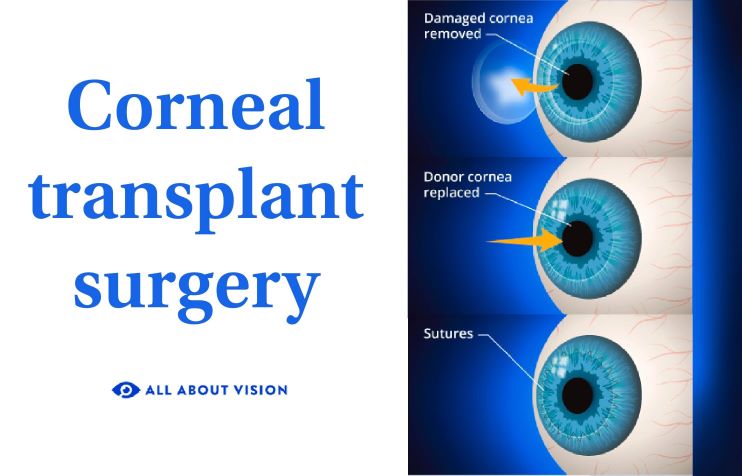
Corneal transplant
A corneal transplant surgery or graft may be necessary when the cornea becomes severely damaged. Conditions that can damage the cornea include corneal infection, inflammation, severe dryness, dystrophies, degenerations and injuries.
Penetrating keratoplasty (PK) – This is a full-thickness cornea transplant. A diseased cornea is replaced with a healthy donor cornea.
Endothelial keratoplasty (EK) – This partial corneal transplant does not need stitches. The back layers of the cornea are replaced. It is performed on patients with corneal dystrophy.
Deep anterior lamellar keratoplasty (DALK) – This procedure replaces the middle tissue layers of the cornea with donor tissue.
Superficial anterior lamellar keratoplasty (SALK) – This procedure replaces the cornea’s outer layers with donor tissue.
Phototherapeutic keratectomy (PTK) – The outermost diseased corneal layers are removed by a laser to allow healthy tissue to regrow.
Retina surgeries
The retina, the light-sensitive tissue at the back of the eye, can be vulnerable to damage and disease. Several types of surgeries exist to treat the retina and its surrounding structures.
Retinal laser photocoagulation
Laser photocoagulation uses a laser to slow down or prevent serious complications that can lead to vision loss. It is used to manage conditions such as diabetic retinopathy, macular edema, retinal vein occlusion, and retinal detachments or tears.
The laser generates heat and creates a burn, stimulating the development of scar tissue. In some cases, the scar tissue is created to help seal off abnormal, leaky blood vessels and reduce swelling.
Unhealthy areas of the retina are sometimes treated with laser photocoagulation to preserve the healthy retina. Retinal holes, tears or small detachments can be “welded” down with this procedure in order to prevent further vision loss.
Photodynamic therapy (PDT)
When the treatment area is near the center of vision, this procedure is preferred over laser photocoagulation to minimize the chances of developing a blind spot. This laser procedure does not cause a heat burn, so the central retina does not get as damaged or scarred as it would with laser photocoagulation. This procedure is commonly used in wet age-related macular degeneration (AMD) patients.
PDT retinal surgery uses a laser and an injected drug that work in combination. The drug is injected into the arm, travels to targeted blood vessels, and is activated by a low-power laser directed at leaky blood vessels. This procedure seals these blood vessels, reducing the amount of fluid and blood they leak.
Cryotherapy
This procedure places a probe that freezes tissue to treat a retinal tear or detachment. The probe damages the tissue surrounding the tear, resulting in a scar that “welds” it into place.
Scleral buckle
A person with a retinal detachment will first be treated with laser photocoagulation or cryotherapy. This is followed by the placement of a scleral buckle — a silicone band placed on the outside of the sclera — to help prevent the retina from detaching again.
This is an outpatient procedure that requires either local or general anesthesia. The surgery lasts for about two hours.
Pneumatic retinopexy
A surgeon may perform an in-office pneumatic retinopexy for retinal detachment, depending on the location of the detachment. After numbing the eye, a small needle is inserted, and some fluid is removed and replaced with a gas bubble. The gas provides gentle pressure against the retina to help it reattach.
This procedure is followed up by laser photocoagulation or cryotherapy to “weld” the retina in place.
Vitrectomy
A vitrectomy removes the vitreous — a gel-like fluid that fills the back two-thirds of the eye — providing support and maintaining its round shape. A vitrectomy is performed for various conditions, such as:
Diabetic retinopathy – To remove blood or scar tissue involving the vitreous and retina
Retinal detachment – To prevent the retina from being pulled away further
Macular pucker – To reduce wrinkling in the area of the macula (central retina)
Macular hole – To prevent the progression of the hole
Endophthalmitis – To treat an infection of the inside of the eyeball
Trauma – To prevent further damage to the eye from an eye injury
This outpatient procedure requires local or general anesthesia and takes a few hours. An incision is made in the eyeball to remove the vitreous and replace it with saline or a bubble of gas and silicone oil.
A patch will be placed over the eye. You will be given medicine to help the eye heal and relieve any mild pain from the procedure. A follow-up appointment to monitor your progress will help your doctor decide when it is safe to return to normal activities.
Eye muscle surgery
Eye muscle surgery helps to align the eyes in a condition called strabismus. This is when the eyes point in different directions, resulting in double vision.
The muscle that needs to be adjusted will be shortened — a resection — or reattached further back in the eye — a recession. Depending on the age of the patient, the procedure may require general anesthesia, although an overnight stay is not usually necessary.
Eyelid surgery
This procedure, called blepharoplasty, repairs eyelids that have become droopy, sometimes impairing vision. It can be performed on both the upper or lower lids. The procedure removes excess skin or fat and can repair the muscle that opens the eyes.
When to see an eye doctor
If your eye doctor recommends that you have eye surgery, it is important to safeguard your eye health and eyesight by following your eye doctor’s recommendations. Routine, comprehensive eye exams are the best way to ensure healthy eyes and clear vision.